• 细胞外基质材料 extracellular matrix materials • 上一篇 下一篇
血管内皮生长因子修饰膀胱脱细胞胶原基质修复尿道缺损
李桂立1,赵启林2
- 1山东医学高等专科学校附属医院,山东省临沂市 276004;2山东大学齐鲁医院泌尿科,山东省济南市 250012
Vascular endothelial growth factor-modified bladder acellular collagen matrix for repair of urethral defects
Li Gui-li1, Zhao Qi-lin2
- 1Affiliated Hospital of Shandong Medical College, Linfen 276004, Shandong Province, China; 2Department of Urology, Qilu Hospital of Shandong University, Jinan 250012, Shandong Province, China
摘要:
文章快速阅读:
.jpg)
文题释义:
膀胱脱细胞胶原基质:采用化学方法去除膀胱壁全层的细胞成分,保留整个膀胱壁的细胞外基质,所得框架机械性能、结构与遗传角度更适于膀胱组织的再生。将其作为移植物支架材料植入组织缺损部位后,能为宿主细胞的增长、生殖提供空间,并在新生组织中不断降解,发挥一种辅助性作用,实现组织器官的内重建。
血管内皮生长因子:又称血管通透因子,是一种高度特异性的促血管内皮细胞生长因子,具有促进血管通透性增加、细胞外基质变性、血管内皮细胞迁移、增殖和血管形成等作用,有5种不同的亚型,根据氨基酸数目分别命名为血管内皮生长因子121、血管内皮生长因子145、血管内皮生长因子165、血管内皮生长因子189、血管内皮生长因子206,其中血管内皮生长因子165为主要存在形式。
背景:研究表明将血管内皮生长因子修饰的膀胱脱细胞胶原基质作为支架用于尿道缺损中,有助于缺损部位修复,促进尿道再生,但不同实验的结果存在争议。
目的:探讨血管内皮生长因子修饰的膀胱脱细胞胶原基质修复家兔尿道缺损的效果。
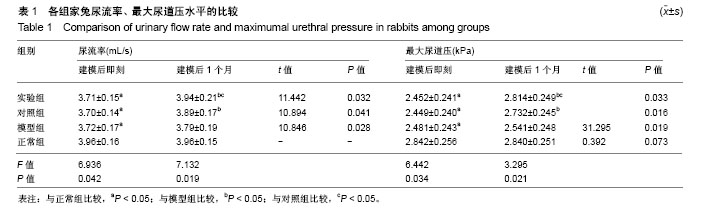
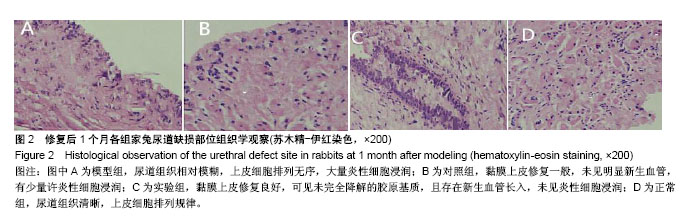
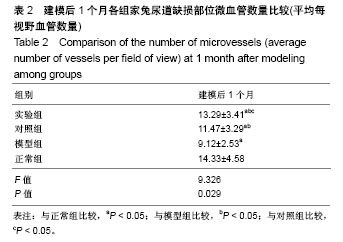
方法:将48只家兔随机分为4组,每组12只,正常组不进行任何处理;模型组、对照组、实验组建立尿道缺损模型,模型建立后即刻,对照组与实验组缺损部位分别植入膀胱脱细胞胶原基质、血管内皮生长因子修饰的膀胱脱细胞胶原基质,模型组不植入任何材料。建模后1个月,检测各组家兔尿流率、最大尿道压,对尿道缺损部位进行苏木精-伊红染色,观察尿道组织修复情况及微血管数量。
结果与结论:①建模后1个月,实验组尿流率、最大尿道压水平高于模型组、对照组(P < 0.05),与正常组比较差异无显著性意义;模型组尿流率、最大尿道压水平低于正常组、对照组(P < 0.05);②建模后1个月,正常组尿道组织清晰,上皮细胞排列规律;模型组尿道组织相对模糊,上皮细胞排列无序,大量炎性细胞浸润;实验组黏膜上皮修复良好,胶原基质部分降解,可见新生血管,未见炎性细胞浸润;对照组黏膜上皮修复一般,未见明显新生血管,少许炎性细胞浸润;③建模后1个月,实验组微血管数量高于其他3组(P < 0.05),对照组微血管数量高于模型组(P < 0.05);④结果表明,采用血管内皮生长因子修饰的膀胱脱细胞胶原基质修复家兔尿道缺损,可促进局部新生血管生成,改善尿道再生所需环境,促进尿道再生。
ORCID: 0000-0002-2796-4809(赵启林)
中图分类号:
.jpg)
.jpg)