中国组织工程研究 ›› 2024, Vol. 28 ›› Issue (6): 840-846.doi: 10.12307/2023.799
• 骨与关节生物力学 bone and joint biomechanics • 上一篇 下一篇
强直性脊柱炎腰椎-骶骨椎间盘有限元模型建立及应力分析
康志杰1,曹振华2,3,许阳阳4,张云凤5,金 凤6,苏宝科7,王利东8,仝 铃1,刘清华1,方 源1,沙丽蓉1,亮 亮9,李濛濛9,
杜奕霏10,林 琳11,王海燕1,李筱贺1,李志军1
- 内蒙古医科大学,1基础医学院人体解剖教研室,10精神卫生学院,内蒙古自治区呼和浩特市 010010;2中国人民解放军总医院骨科,北京市 100853;内蒙古医科大学第二附属医院,3微创脊柱外科,5影像科,内蒙古自治区呼和浩特市 010010;4山西省长治市人民医院康复医学科,山西省长治市 046000;6内蒙古医科大学附属医院影像科,内蒙古自治区呼和浩特市 010010;7内蒙古自治区中医医院,内蒙古自治区呼和浩特市 010010;8内蒙古自治区国际蒙医医院,内蒙古自治区呼和浩特市 010010;9内蒙古医科大学第一临床医学院,内蒙古自治区呼和浩特市 010010;11内蒙古医科大学附属人民医院,内蒙古自治区呼和浩特市 010010
Finite element model establishment and stress analysis of lumbar-sacral intervertebral disc in ankylosing spondylitis
Kang Zhijie1, Cao Zhenhua2, 3, Xu Yangyang4, Zhang Yunfeng5, Jin Feng6, Su Baoke7, Wang Lidong8, Tong Ling1, Liu Qinghua1, Fang Yuan1, Sha Lirong1, Liang Liang9, Li Mengmeng9, Du Yifei10, Lin Lin11, Wang Haiyan1, Li Xiaohe1, Li Zhijun1
- 1Department of Human Anatomy, School of Basic Medicine, 10Mental Health School, Inner Mongolia Medical University, Hohhot 010010, Inner Mongolia Autonomous Region, China; 2Department of Orthopedics, Chinese People’s Liberation Army General Hospital, Beijing 100853, China; 3Department of Minimally Invasive Spine Surgery, 5Department of Imaging, Second Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010010, Inner Mongolia Autonomous Region, China; 4Department of Rehabilitation Medicine, Changzhi People’s Hospital, Changzhi 046000, Shanxi Province, China; 6Department of Imaging, Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010010, Inner Mongolia Autonomous Region, China; 7Inner Mongolia Hospital of Traditional Chinese Medicine, Hohhot 010010, Inner Mongolia Autonomous Region, China; 8Inner Mongolia International Mongolian Hospital, Hohhot 010010, Inner Mongolia Autonomous Region, China; 9First Clinical Medical College of Inner Mongolia Medical University, Hohhot 010010, Inner Mongolia Autonomous Region, China; 11Affiliated People’s Hospital of Inner Mongolia Medical University, Hohhot 010010, Inner Mongolia Autonomous Region, China
摘要:
文题释义:
强直性脊柱炎:属于一种风湿免疫类疾病,是以脊柱为主要病变部位的慢性炎症疾病,其病因尚不清楚,常累及骶髂关节,最终引起脊柱强直和纤维化,呈现“竹脊柱”样改变,并伴有不同程度的眼、肺、肠道、心血管等关节外器官的病变。有限元分析:是指利用数学方法模拟真实的几何和载荷工况,可将实际连续的离散单元集合到一起,采用简单而又相互作用的单元使复杂问题简单化,最终得到问题结果的一种高效、实用的数值分析方式。由于有限元分析方便、有效、实用,已被应用于所有科学技术领域。
背景:强直性脊柱炎是一种风湿免疫类慢性炎症反应疾病,软组织骨化融合及脊柱强直可致生物力学改变。
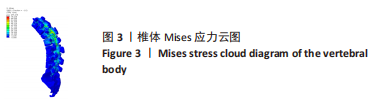
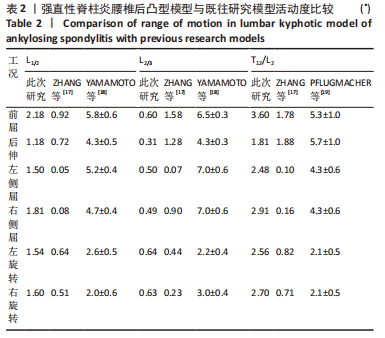
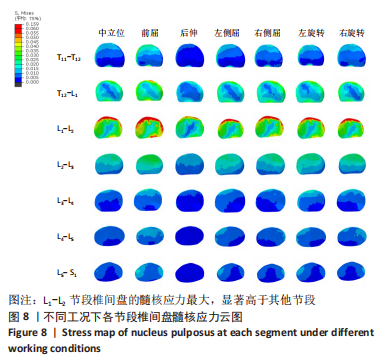
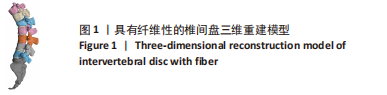
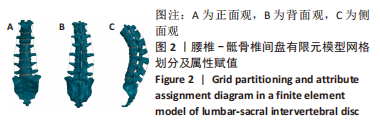
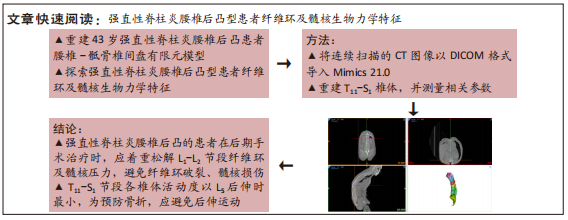
目的:利用有限元分析方法重建强直性脊柱炎腰椎后凸患者的腰椎-骶骨椎间盘,研究T11-S1节段各椎体活动度及纤维环、髓核的生物力学特征。方法:获取1例强直性脊柱炎腰椎后凸患者的影像资料,将连续扫描的脊柱CT原始影像数据以 DICOM 格式导入Mimics 21.0,分别重建T11-S1。随后将建立好的模型以“Stl”格式导入3-Matic软件进行椎间盘的重建,得到具有纤维性的椎间盘模型。将完善的模型继续导入Hypermesh 软件,对椎体、髓核、纤维环、韧带进行网格划分,赋予材料属性后将模型导入ABAQUS软件中,观察T11-S1各椎体在不同工况下的活动度,并分析各节段纤维环及髓核的生物力学特征。
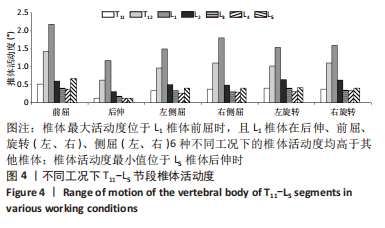
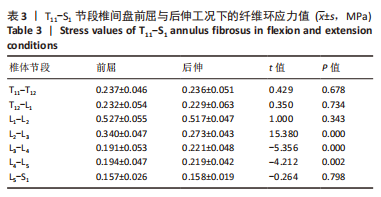
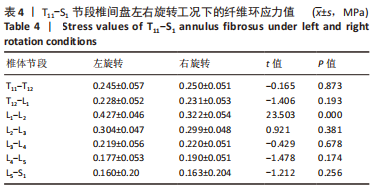
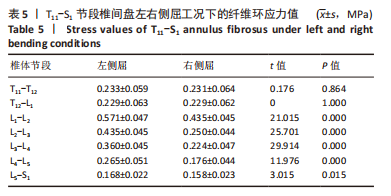
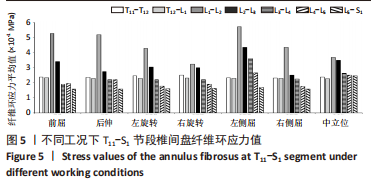
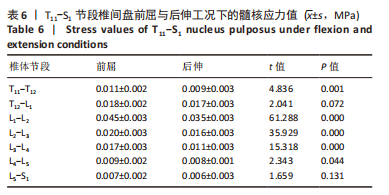
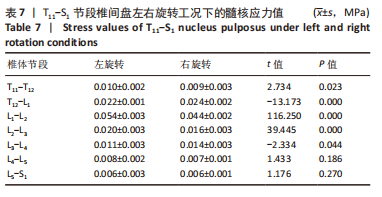
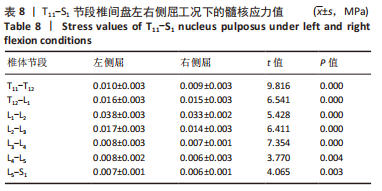
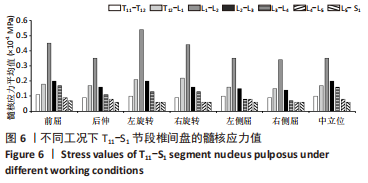
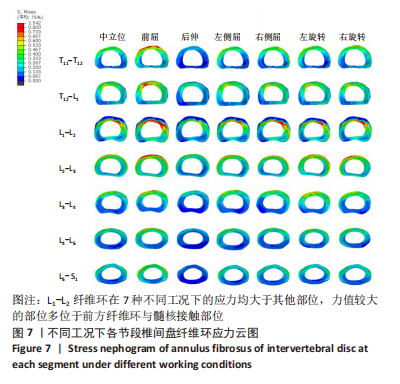
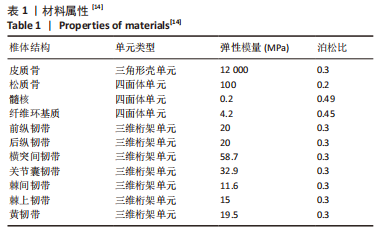
结果与结论:①L1节段在后伸、前屈、旋转(左、右)、侧屈(左、右)工况下的活动度均大于其他椎体,L1椎体前屈时的活动度最大,为2.18°;L5节段后伸工时的活动度最小,为0.12°;②L2-L3节段椎间盘前屈时的纤维环应力大于后伸时(P < 0.05),L3-L4、L4-L5节段椎间盘前屈时的纤维环应力小于后伸时(P < 0.05),L1-L2节段椎间盘左旋转时的纤维环应力大于右旋转时(P < 0.05),L1-L2、L2-L3、L3-L4、L4-L5、L5-S1节段椎间盘左侧屈时的纤维环应力大于右侧屈时(P < 0.05);③T11-L12、L1-L2、L2-L3、L3-L4、L4-L5节段前屈时的髓核应力大于后伸时(P < 0.05),T12-L1、L3-L4节段椎间盘左旋转时的髓核应力小于右旋转时(P < 0.05),T11-T12、L1-L2、L2-L3节段椎间盘左旋转时的髓核应力大于右旋转时(P < 0.05),T11-S1节段椎间盘左侧屈时的髓核应力均大于右侧屈时;④结果显示,强直性脊柱炎腰椎后凸患者椎体活动度最小值位于后伸工况下的L5椎体,为预防骨折建议避免后伸体位的运动;强直性脊柱炎腰椎后凸患者发病时,纤维环及髓核最大应力部位在L1-L2节段,部位固定且不会随体位的改变而变化,后期手术治疗、矫正畸形应着重松解该节段纤维环及髓核的压力,避免纤维环破裂、髓核损伤。
https://orcid.org/0000-0001-6025-7535 (康志杰);https://orcid.org/0000-0003-0663-7339 (曹振华)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号: