| [1] 段钟平,陈煜.肝衰竭诊疗: 进展与展望[J].临床肝胆病杂志, 2012, 28(10):721-725.[2] 中华医学会感染病学分会肝衰竭与人工肝学组,中华医学会肝病学分会重型肝病与人工肝学组.肝衰竭诊治指南[J].中华临床感染病杂志,2012,5(6):321-327.[3] 叶一农,高志良.乙型肝炎肝衰竭发生机制中的三重打击[J].传染病信息,2009,22(5):276-279.[4] 中华医学会肝病学分会重型肝病与人工肝学组,中华医学会感染病学分会肝衰竭与人工肝学组.肝衰竭诊疗指南[J].中华肝脏病杂志, 2006,14(9):643-646.[5] Mabuchi A,Mullaney I,Sheard P,et al.Role of hepatic stellate cells in the early phase of liver regeneration in rat: formation of tight adhesion to parenchymal cells.Comp Hepatol.2004;3 Suppl 1:S29.[6] Cohn R,Herrod C.Some effects upon the liver of complete arterialization of its blood supply. Surgery.1952;32(2):214.[7] Fisher B,Russ C,Updegraff H.A suitable technique for total arterialization of the dog liver.Surgery.Surgery. 1954;35(6): 879-884.[8] Schleimer K,Stippel DL,Kasper HU,et al.Improved microcirculation of a liver graft by controlled portal vein arterialization.J Surg Res.2004;116(2):202-210.[9] Margarit C,Bilbao I,Charco R,et al.Auxiliary heterotopic liver transplantation with portal vein arterialization for fulminant hepatic failure.Liver Transpl.2000;6(6):805-809.[10] 刘琦,李坚,关晓东,等.入肝门静脉动脉化加门腔分流术对肝硬化大鼠血流动力学的影响[J].中华普通外科学文献(电子版),2010,4(2):16-19.[11] Schleimer K,Stippel DL,Kasper HU,et al.Auxiliary liver transplantation with flow‐regulated portal vein arterialization offers a successful therapeutic option in acute hepatic failure–investigations in heterotopic auxiliary rat liver transplantation. Transplant Int.2006;19(7): 581-588.[12] 陈永亮,黄晓强,黄志强,等.部分门静脉动脉化对大鼠肝脏血管铸型变化的影[J].中国普通外科杂志,2007,16(3):223-226.[13] Fernández OM,Ríos A,Sánchez A,et al.Pathology findings in a model of auxiliary liver transplantation with portal vein arterialization in pigs.Transplant Proc.2005;37(9):3939-3942.[14] Nardo B,Montalti R,Puviani L,et al.Portal vein oxygen supply through a liver extracorporeal device to treat acute liver failure in Swine induced by subtotal hepatectomy: preliminary data. Transplant Proc.2006;38(4):1190-1192.[15] Nardo B,Tsivian M,Neri F,et al.Extracorporeal portal vein oxygenation improves outcome of acute liver failure in swine. Transplant Proc.2008;40(6):2046-2048. [16] Tsivian M,Neri F,Prezzi D,et al.Portal vein arterialization in hepatobiliary surgery and liver transplantation.Transplantation proceedings.Elsevier.2007;39(6):1877-1878.[17] Schleimer K,Stippel DL,Kasper HU,et al.Portal vein arterialization increases hepatocellular apoptosis and inhibits liver regeneration. J Surg Res.2008;149(2):250-258.[18] Muller V,Ott R,Tannapfel A,et al.Arterialization of the portal vein in liver transplantation: a new microsurgical model in the rat. Transplantation.2001;71(7):977-981.[19] Schleimer K,Stippel DL,Kasper HU,et al.Portal hyperperfusion causes disturbance of microcirculation and increased rate of hepatocellular apoptosis: investigations in heterotopic rat liver transplantation with portal vein arterialization.Transplant Proc. 2006;38(3):725-729.[20] Seifter S,England S.Energy metabolism. In: Arias IM,et al (eds).The liver: biology and pathobiology, 3rd edn.Raven Press, New York,1994:323-364.[21] Bonnet S,Sauvanet A,Bruno O,et al.Long-term survival after portal vein arterialization for portal vein thrombosis in orthotopic liver transplantation.Gastroenterol Clin Biol.2010;34(1):23-28. [22] Pastor CM.Hepatic and splanchnic oxygen consumption during acute hypoxemic hypoxia in anesthetized pigs.Crit Care Med. 2000;28(3):765-773.[23] Stieber AC,Zetti G,Todo S,et al.The spectrum of portal vein thrombosis in liver transplantation.Ann Surg.1991;213(3):199.[24] Fan YD,Praet M,Van Huysse J,et al.Effects of portal vein arterialization on liver regeneration after partial hepatectomy in the rat.Liver Transpl.2002;8(2):146-152.[25] Kruel CRP,de Fraga RS,Dal Molin S,et al.Hepatic reperfusion in rats: a new model with portal arterialization in studying early ischemia-reperfusion injury.Transplant Proc. 2007;39(10): 3015-3018.[26] Schleimer K,Stippel DL,Kasper HU,et al.Improved microcirculation of a liver graft by controlled portal vein arterialization.J Surg Res.2004;116(2):202-210.[27] 陈永亮,黄志强,王迎宾,等.门静脉动脉化对实验性梗阻性黄疸大鼠肝细胞凋亡的影响[J].中华普通外科杂志,2000,15(6):348-351.[28] 吴均政,江艺,张小进,等.一种新的大鼠门静脉动脉化模型[J].中国组织工程研究,2011,15(15):2716-2720.[29] 李兰娟,肖党生,吴仲文,等.急性肝衰竭大鼠肠道菌群和内毒素的动态研究[J].中华肝脏病杂志,2004,12(3):167-169. [30] Takenaka K,Kanematsu T,Fukuzawa K,et al.Can hepatic failure after surgery for hepatocellular carcinoma in cirrhotic patients be prevented? World J Surg.1990;14(1):123-127.[31] Pugh RNH,Murray-Lyon IM,Dawson JL,et al.Transection of the oesophagus for bleeding oesophageal varices.Br J Surg.1973; 60(8):646-649.[32] Van Deventer SJ,Ten Cate JW,Tytgat GN.Intestinal endotoxemia. Clinical significanc. Gastroenterology.1988;94(3):825.[33] 李兰娟,肖党生,吴仲文,等.急性肝衰竭大鼠肠道菌群和内毒素的动态研究[J].中华肝脏病杂志,2004, 12(3):167-169.[34] Steuerwald NM,Foureau DM,Norton HJ,et al.Profiles of serum cytokines in acute drug-induced liver injury and their prognostic significance.PloS One.2013;8(12):e81974.[35] Chastre A,Bélanger M,Beauchesne E,et al.Inflammatory cascades driven by tumor necrosis factor-alpha play a major role in the progression of acute liver failure and its neurological complications.PloS One.2012;7(11):e49670.[36] Schwabe RF,Brenner DA.Mechanisms of liver injury. I. TNF-α-induced liver injury: role of IKK, JNK, and ROS pathways.Am J Physiol Gastrointest Liver Physiol.2006;290(4):G583-589.[37] Lai HS,Lin WH,Lai SL,et al.Interleukin-6 mediates angiotensinogen gene expression during liver regeneration.PloS One.2013;8(7):e67868.[38] Han Y,Runge MS,Brasier AR.Angiotensin II induces interleukin-6 transcription in vascular smooth muscle cells through pleiotropic activation of nuclear factor-κB transcription factors.Circ Res. 1999;84(6):695-703. |
.jpg) 文题释义:
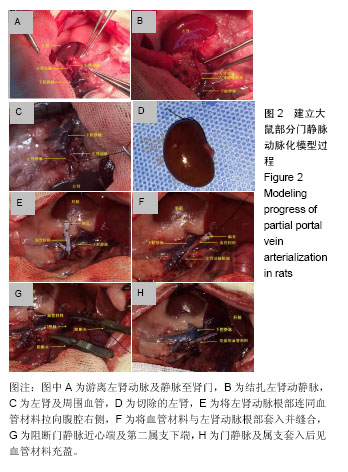
门静脉动脉化:是指通过腹腔内便于应用的动脉将动脉血引入门静脉,通过提高门静脉血供改善肝脏功能的方法。20世纪50年代,Cohn(1952年)和Fisher(1954年)为增加门腔分流术后导致的肝脏血流灌注不足、改善肝功能,首次提出门静脉动脉化这一创新理念,目前已将其应用于肝移植、肝门部胆管肿瘤、胰腺肿瘤、胆囊肿瘤、各种原因导致的门静脉高压门体分流 等手术中,特别是对于肝移植、肝门部胆管肿瘤和胆囊肿瘤,有较多成功案例报道。
文题释义:
门静脉动脉化:是指通过腹腔内便于应用的动脉将动脉血引入门静脉,通过提高门静脉血供改善肝脏功能的方法。20世纪50年代,Cohn(1952年)和Fisher(1954年)为增加门腔分流术后导致的肝脏血流灌注不足、改善肝功能,首次提出门静脉动脉化这一创新理念,目前已将其应用于肝移植、肝门部胆管肿瘤、胰腺肿瘤、胆囊肿瘤、各种原因导致的门静脉高压门体分流 等手术中,特别是对于肝移植、肝门部胆管肿瘤和胆囊肿瘤,有较多成功案例报道。.jpg) 文题释义:
门静脉动脉化:是指通过腹腔内便于应用的动脉将动脉血引入门静脉,通过提高门静脉血供改善肝脏功能的方法。20世纪50年代,Cohn(1952年)和Fisher(1954年)为增加门腔分流术后导致的肝脏血流灌注不足、改善肝功能,首次提出门静脉动脉化这一创新理念,目前已将其应用于肝移植、肝门部胆管肿瘤、胰腺肿瘤、胆囊肿瘤、各种原因导致的门静脉高压门体分流 等手术中,特别是对于肝移植、肝门部胆管肿瘤和胆囊肿瘤,有较多成功案例报道。
文题释义:
门静脉动脉化:是指通过腹腔内便于应用的动脉将动脉血引入门静脉,通过提高门静脉血供改善肝脏功能的方法。20世纪50年代,Cohn(1952年)和Fisher(1954年)为增加门腔分流术后导致的肝脏血流灌注不足、改善肝功能,首次提出门静脉动脉化这一创新理念,目前已将其应用于肝移植、肝门部胆管肿瘤、胰腺肿瘤、胆囊肿瘤、各种原因导致的门静脉高压门体分流 等手术中,特别是对于肝移植、肝门部胆管肿瘤和胆囊肿瘤,有较多成功案例报道。
.jpg) 文题释义:
门静脉动脉化:是指通过腹腔内便于应用的动脉将动脉血引入门静脉,通过提高门静脉血供改善肝脏功能的方法。20世纪50年代,Cohn(1952年)和Fisher(1954年)为增加门腔分流术后导致的肝脏血流灌注不足、改善肝功能,首次提出门静脉动脉化这一创新理念,目前已将其应用于肝移植、肝门部胆管肿瘤、胰腺肿瘤、胆囊肿瘤、各种原因导致的门静脉高压门体分流 等手术中,特别是对于肝移植、肝门部胆管肿瘤和胆囊肿瘤,有较多成功案例报道。
文题释义:
门静脉动脉化:是指通过腹腔内便于应用的动脉将动脉血引入门静脉,通过提高门静脉血供改善肝脏功能的方法。20世纪50年代,Cohn(1952年)和Fisher(1954年)为增加门腔分流术后导致的肝脏血流灌注不足、改善肝功能,首次提出门静脉动脉化这一创新理念,目前已将其应用于肝移植、肝门部胆管肿瘤、胰腺肿瘤、胆囊肿瘤、各种原因导致的门静脉高压门体分流 等手术中,特别是对于肝移植、肝门部胆管肿瘤和胆囊肿瘤,有较多成功案例报道。