中国组织工程研究 ›› 2019, Vol. 23 ›› Issue (7): 990-995.doi: 10.3969/j.issn.2095-4344.1063
• 骨组织构建 bone tissue construction • 上一篇 下一篇
骨密度测试联合老年人运动功能量表-25评估筛查老年人基础运动障碍及跌倒风险:天津市6个社区1 458例调查
宋 超1,田 鑫1,刘 琳1,徐雅雯1,孟 圆1,李晓丽1,彭 萌2,李华东2,王志涛3,戈 莎1
- (天津师范大学,1体育科学学院, 2体育竞赛训练中心,天津市 300387;3天津医科大学总医院神经外科,天津市 300052)
Application of 25-question Geriatric Locomotive Function Scale combined with bone mineral density test in screening locomotive syndrome and risk of falls in the elderly: a survey of 1 458 people from 6 urban communities in Tianjin
Song Chao1, Tian Xin1, Liu Lin1, Xu Yawen1, Meng Yuan1, Li Xiaoli1, Peng Meng2, Li Huadong2, Wang Zhitao3, Ge Sha1
- (1College of Sports Science, Tianjin Normal University, Tianjin 300387, China; 2Sports Competition Training Center, Tianjin Normal University, Tianjin 300387, China; 3Department of Neurosurgery, General Hospital Affiliated to Tianjin Medical University, Tianjin 300052, China)
摘要:
文章快速阅读:
.jpg) 文题释义:
运动障碍:随意运动兴奋、抑制或不能由意志控制的现象,常见于神经系统疾病、精神障碍、创伤等。运动功能有随意运动和不随意运动两类。随意运动是有意识的,能随自己的意志进行的运动,又称自主运动。不随意运动指内脏运动神经和血管运动神经所支配的心肌、平滑肌的运动,是不经意识、不受自己意志控制的运动。一般所说运动指随意运动而言。运动神经系统指锥体系统、锥体外系(纹状体-苍白球系统)和皮质-脑桥-小脑系统,而由周围运动神经元发出冲动控制骨骼肌的活动。
风险评估(Risk Assessment):是指在风险事件发生之前或之后(但还没有结束),该事件给人们的生活、生命、财产等各个方面造成的影响和损失的可能性进行量化评估的工作。即,风险评估就是量化测评某-事件或事物带来的影响或损失的可能程度。
文题释义:
运动障碍:随意运动兴奋、抑制或不能由意志控制的现象,常见于神经系统疾病、精神障碍、创伤等。运动功能有随意运动和不随意运动两类。随意运动是有意识的,能随自己的意志进行的运动,又称自主运动。不随意运动指内脏运动神经和血管运动神经所支配的心肌、平滑肌的运动,是不经意识、不受自己意志控制的运动。一般所说运动指随意运动而言。运动神经系统指锥体系统、锥体外系(纹状体-苍白球系统)和皮质-脑桥-小脑系统,而由周围运动神经元发出冲动控制骨骼肌的活动。
风险评估(Risk Assessment):是指在风险事件发生之前或之后(但还没有结束),该事件给人们的生活、生命、财产等各个方面造成的影响和损失的可能性进行量化评估的工作。即,风险评估就是量化测评某-事件或事物带来的影响或损失的可能程度。
.jpg) 文题释义:
运动障碍:随意运动兴奋、抑制或不能由意志控制的现象,常见于神经系统疾病、精神障碍、创伤等。运动功能有随意运动和不随意运动两类。随意运动是有意识的,能随自己的意志进行的运动,又称自主运动。不随意运动指内脏运动神经和血管运动神经所支配的心肌、平滑肌的运动,是不经意识、不受自己意志控制的运动。一般所说运动指随意运动而言。运动神经系统指锥体系统、锥体外系(纹状体-苍白球系统)和皮质-脑桥-小脑系统,而由周围运动神经元发出冲动控制骨骼肌的活动。
风险评估(Risk Assessment):是指在风险事件发生之前或之后(但还没有结束),该事件给人们的生活、生命、财产等各个方面造成的影响和损失的可能性进行量化评估的工作。即,风险评估就是量化测评某-事件或事物带来的影响或损失的可能程度。
文题释义:
运动障碍:随意运动兴奋、抑制或不能由意志控制的现象,常见于神经系统疾病、精神障碍、创伤等。运动功能有随意运动和不随意运动两类。随意运动是有意识的,能随自己的意志进行的运动,又称自主运动。不随意运动指内脏运动神经和血管运动神经所支配的心肌、平滑肌的运动,是不经意识、不受自己意志控制的运动。一般所说运动指随意运动而言。运动神经系统指锥体系统、锥体外系(纹状体-苍白球系统)和皮质-脑桥-小脑系统,而由周围运动神经元发出冲动控制骨骼肌的活动。
风险评估(Risk Assessment):是指在风险事件发生之前或之后(但还没有结束),该事件给人们的生活、生命、财产等各个方面造成的影响和损失的可能性进行量化评估的工作。即,风险评估就是量化测评某-事件或事物带来的影响或损失的可能程度。摘要
背景:老年人运动功能量表(geriatric locomotive function scale,GLFS)-25、平衡功能评定、步态测试等常用于筛查老年人运动功能障碍和预测跌倒风险的方法均属于主观评定方法,因此结合客观的评价指标能更为全面地反映老年人的运动功能状态和平衡功能。
目的:探讨GLFS-25量表联合骨密度测试在筛查天津市6个社区老年人基础运动障碍和评估患者跌倒风险中的应用效果。
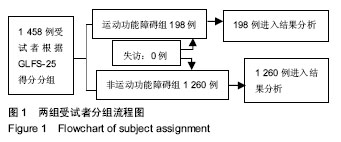
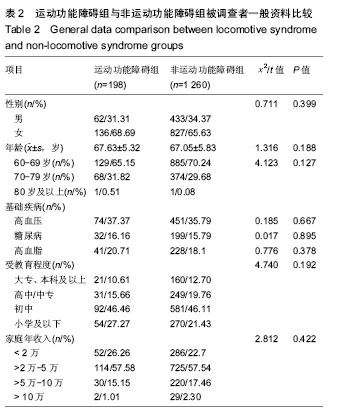
方法:采用分区整群随机抽样调查法抽取天津市和平区、南开区的6个社区老年人1 458例进行调查,根据GLFS-25得分情况将其分为运动功能障碍组(198例,GLFS-25≥16分)和非运动功能障碍组(1 260例,GLFS-25<16分)。比较两组调查对象的身高、体质量、体质量指数、体脂肪率、内脏脂肪面积等相关因素,比较两组受试者骨密度、跌倒次数、膝关节灵活度和下肢力量、平衡功能评分及步态分析,并进行相关性分析;采用受试者工作特征曲线分析GLFS-25联合骨密度测试诊断老年人基础运动障碍及跌倒风险的效能。
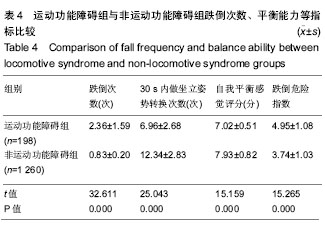
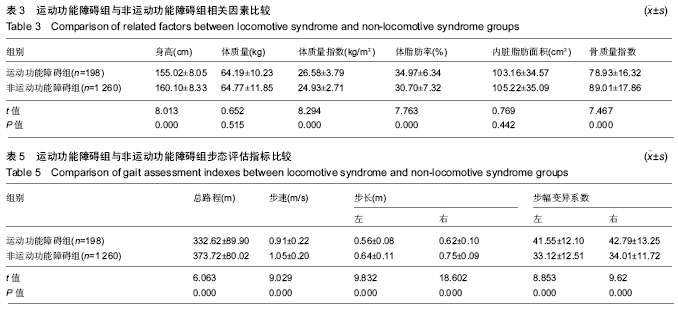
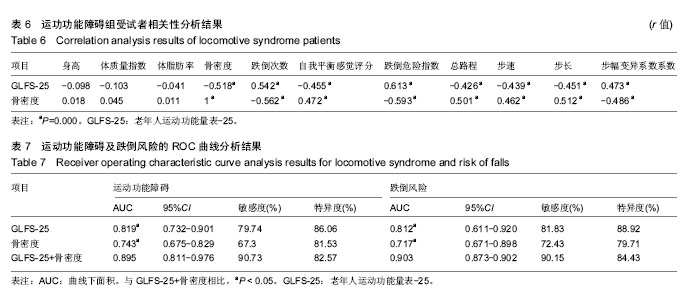
结果与结论:①运动功能障碍组身高显著低于非运动功能障碍组、体质量指数和体脂肪率显著高于非运动功能障碍组(P < 0.05),运动功能障碍组骨密度值显著低于非运动功能障碍组(t=7.467,P=0.000);②非运动功能障碍组的过去1年平均跌倒次数和跌倒危险指数显著低于运动功能障碍组,30 s内坐立姿势转换次数、自我平衡感觉评分显著高于运动功能障碍组(P均为0.000);非运动功能障碍组的总路程、平均步速、左右平均步长均显著高于运动功能障碍组,其左右步幅变异系数均显著低于运动障碍组 (P < 0.05);③Pearson相关性分析结果显示,GLFS-25评分、骨密度与身高、体质量指数和体脂肪率无明显相关性(P > 0.05),GLFS-25评分与骨密度、自我平衡感觉、总路程、平均步速、左右平均步长均呈负相关,与跌倒次数、跌倒危险指数、左右步幅变异系数呈正相关(P < 0.05);④受试者工作特征曲线曲线分析显示,GLFS-25联合骨密度预测运动功能障碍及跌倒风险的曲线下面积分别为0.895和0.903,均显著高于GLFS25和骨密度单独检测,其灵敏度分别提高至90.73%和90.15%;⑤结果说明,天津市市区社区老年人存在基础运动功能障碍者的比例较高,运动功能障碍患者的GLFS-25评分更高、骨密度更低,由于其膝关节灵活度和下肢力量及平衡能力更差,跌倒风险相应也更高,而GLFS-25联合骨密度测试在老年人基础运动障碍的筛查和跌倒风险评估预测中的效能更优。
中国组织工程研究杂志出版内容重点:组织构建;骨细胞;软骨细胞;细胞培养;成纤维细胞;血管内皮细胞;骨质疏松;组织工程
ORCID: 0000-0001-5886-2779(宋超)
中图分类号:

.jpg) 文题释义:
运动障碍:随意运动兴奋、抑制或不能由意志控制的现象,常见于神经系统疾病、精神障碍、创伤等。运动功能有随意运动和不随意运动两类。随意运动是有意识的,能随自己的意志进行的运动,又称自主运动。不随意运动指内脏运动神经和血管运动神经所支配的心肌、平滑肌的运动,是不经意识、不受自己意志控制的运动。一般所说运动指随意运动而言。运动神经系统指锥体系统、锥体外系(纹状体-苍白球系统)和皮质-脑桥-小脑系统,而由周围运动神经元发出冲动控制骨骼肌的活动。
风险评估(Risk Assessment):是指在风险事件发生之前或之后(但还没有结束),该事件给人们的生活、生命、财产等各个方面造成的影响和损失的可能性进行量化评估的工作。即,风险评估就是量化测评某-事件或事物带来的影响或损失的可能程度。
文题释义:
运动障碍:随意运动兴奋、抑制或不能由意志控制的现象,常见于神经系统疾病、精神障碍、创伤等。运动功能有随意运动和不随意运动两类。随意运动是有意识的,能随自己的意志进行的运动,又称自主运动。不随意运动指内脏运动神经和血管运动神经所支配的心肌、平滑肌的运动,是不经意识、不受自己意志控制的运动。一般所说运动指随意运动而言。运动神经系统指锥体系统、锥体外系(纹状体-苍白球系统)和皮质-脑桥-小脑系统,而由周围运动神经元发出冲动控制骨骼肌的活动。
风险评估(Risk Assessment):是指在风险事件发生之前或之后(但还没有结束),该事件给人们的生活、生命、财产等各个方面造成的影响和损失的可能性进行量化评估的工作。即,风险评估就是量化测评某-事件或事物带来的影响或损失的可能程度。