中国组织工程研究 ›› 2016, Vol. 20 ›› Issue (32): 4751-4757.doi: 10.3969/j.issn.2095-4344.2016.32.006
• 肿瘤干细胞 cancer stem cells • 上一篇 下一篇
内分泌和化疗对乳腺肿瘤患者干细胞的影响
赵艳丽1,刁建华2,吴彩琴1,张彩霞1,贾焕霞1,牛朝霞3
- 1许昌学院医学院,河南省许昌市 461000
2许昌市中心医院内分泌科,河南省许昌市 461000
3河南医学高等专科学校病理生理学教研室,河南省郑州市 451191
Effects of endocrine therapy and chemotherapy on stem cells in patients with breast cancer
Zhao Yan-li1, Diao Jian-hua2, Wu Cai-qin1, Zhang Cai-xia1, Jia Huan-xia1, Niu Zhao-xia3
- 1School of Medicine of Xuchang University, Xuchang 461000, Henan Province, China
2Department of Endocrinology, Xuchang Municipal Central Hospital, Xuchang 461000, Henan Province, China
3Department of Pathophysiology, Henan Medical College, Zhengzhou 451191, Henan Province, China
摘要:
文章快速阅读:
.jpg)
文题释义: 乳腺癌内分泌治疗:经历了100多年的演变,已发展成为雌激素受体阳性乳腺癌患者不可或缺的治疗手段。因此,雌激素及抗雌激素药物对雌激素受体阳性乳腺癌患者肿瘤干细胞的作用至关重要,因为其直接决定着乳腺癌患者内分泌治疗的疗效。 肿瘤干细胞:肿瘤组织内部有一群含量很低的细胞,可以在分化为肿瘤细胞的同时保持干细胞样功能。大多数细胞毒性药物和放射治疗肿瘤的机制都是阻滞处于分裂期的细胞,虽然可以杀灭大量的肿瘤细胞,但长期处于静止状态的肿瘤干细胞却可以逃避药物的杀伤作用,这部分细胞在肿瘤复发、转移中起着重要作用。
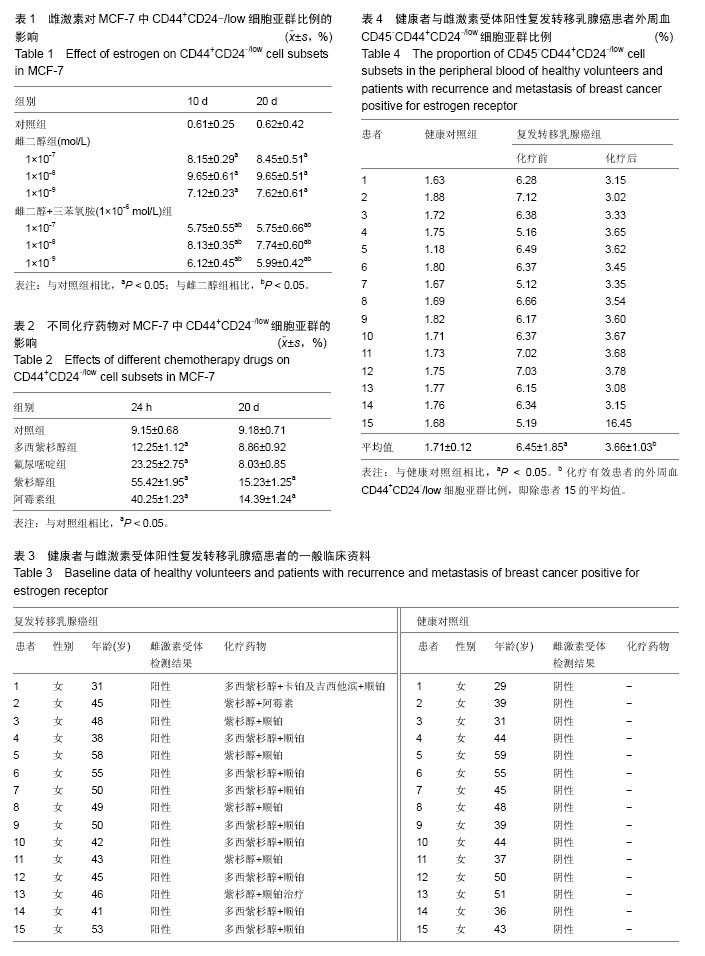
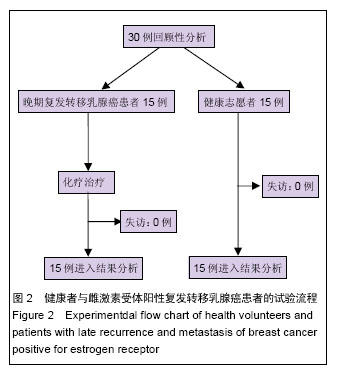
摘要 背景:肿瘤干细胞是恶性肿瘤复发及转移的根源,不同治疗方法对肿瘤中肿瘤干细胞的影响是临床研究的重点。 目的:探讨内分泌和化疗对乳腺肿瘤患者干细胞的影响。 方法:①对雌激素受体阳性人乳腺癌细胞株 MCF-7进行复苏和培养,选取第3代对数期细胞分为对照组、雌二醇组和雌二醇+三苯氧胺组。对照组培养基中添加等量无水乙醇,雌二醇组分为1×10-7,1×10-8,1×10-9 mol/L三个亚组,分别在培养基中加入1×10-7,1×10-8,1×10-9 mol/L雌二醇。雌二醇+三苯氧胺组按雌二醇浓度的差异分为三个亚组,培养基中分别加入1×10-7,1×10-8,1×10-9 mol/L雌二醇,3个亚组均同时加入1×10-6 mol/L的三苯氧胺。②晚期复发转移乳腺癌女性患者15例为雌激素受体阳性复发转移乳腺癌组,接受化疗治疗。另取15名健康志愿者作为健康对照组。 结果与结论:①雌二醇组和雌二醇+三苯氧胺组CD44+CD24-/low细胞亚群比例均显著高于对照组(P < 0.05),雌二醇组CD44+CD24-/low细胞亚群比例显著高于同浓度雌二醇+三苯氧胺组(P < 0.05)。各组培养10 d和20 d时的CD44+CD24-/low细胞亚群比例接近(P > 0.05)。②不同化疗药物均对MCF-7细胞的增殖产生一定的抑制作用,且呈现出剂量-效应依赖现象。MCF-7经不同化疗药物干预24 h后,细胞中CD44+CD24-/low细胞亚群的比例均明显增加(P < 0.05);但干预20 d后仅紫杉醇和阿霉素组细胞中CD44+CD24-/low细胞亚群比例高于对照组(P < 0.05)。③健康者外周血CD44+CD24-/low细胞亚群比例显著低于雌激素受体阳性复发转移乳腺癌患者(P < 0.05)。在15例雌激素受体阳性复发转移乳腺癌患者中,9例疾病稳定,5例部分缓解,1 例化疗无效,疾病进展。化疗有效者化疗后的外周血CD45-CD44+CD24-/low细胞亚群比例均显著低于化疗前(P < 0.05)。⑤结果说明内分泌治疗与化疗会对雌激素受体阳性乳腺癌的CD44+CD24-/low细胞亚群产生一定的影响。MCF-7细胞中CD44+CD24-/low细胞亚群会对一定的化疗药物产生抵抗能力,经化疗有效的患者外周血CD45-CD44+CD24-/low细胞比例会出现下降。
中图分类号:
.jpg)
.jpg)