中国组织工程研究 ›› 2015, Vol. 19 ›› Issue (6): 883-890.doi: 10.3969/j.issn.2095-4344.2015.06.011
• 干细胞移植 stem cell transplantation • 上一篇 下一篇
骨髓间充质干细胞移植联合髓芯减压植骨修复股骨头坏死
张 洋,王 楠,杨立枫,马 骥,李 治
- 沈阳医学院附属中心医院,辽宁省沈阳市 110024
-
出版日期:2015-02-05发布日期:2015-02-05 -
通讯作者:李治,吉林大学在读博士,主任医师,沈阳医学院附属中心医院,辽宁省沈阳市 110024 -
作者简介:张洋,男,1981年生,辽宁省沈阳市人,汉族,2011年中国医科大学毕业,硕士,主治医师,主要从事脊柱以及关节骨病的基础与临床研究。
Bone marrow mesenchymal stem cell transplantation combined with core decompression and bone grafting in the repair of osteonecrosis of femoral head
Zhang Yang, Wang Nan, Yang Li-feng, Ma Ji, Li Zhi
- Central Hospital Affiliated to Shenyang Medical College, Shenyang 110024, Liaoning Province, China
-
Online:2015-02-05Published:2015-02-05
摘要:
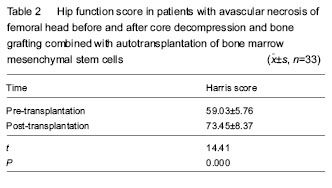
背景:单独使用髓芯减压治疗股骨头坏死,易造成股骨头凹陷和内部显微结构的崩溃,因而需要自体骨等材料进行填充支撑,而骨髓干细胞移植能使股骨头塌陷的发生率降低。 目的:观察髓芯减压植骨联合骨髓间充质干细胞移植治疗股骨头坏死的临床效果。 方法:选择2012年12月至2013年5月在沈阳医学院附属中心医院骨外四科住院的33例采用股骨头髓芯减压植骨联合骨髓间充质干细胞注入髓腔内治疗股骨头坏死患者。 结果与结论:股骨头髓芯减压植骨联合骨髓间充质干细胞注入髓腔内治疗股骨头坏死后患者Harris髋关节功能评分增加,疼痛消失,能从事各种劳动;X射线片或CT检查显示股骨头正常30髋,占79%;疼痛明显减轻,行走基本正常或者轻微跛行15髋,占40%;行走间距延长35髋,占92%;髋关节功能障碍明显好转24髋,占63%。提示髓芯减压植骨联合骨髓间充质干细胞移植对改善股骨头缺血性坏死局部血供,促进坏死骨质吸收和骨质修复起到积极的作用。
中图分类号:
引用本文
张 洋,王 楠,杨立枫,马 骥,李 治. 骨髓间充质干细胞移植联合髓芯减压植骨修复股骨头坏死[J]. 中国组织工程研究, 2015, 19(6): 883-890.
Zhang Yang, Wang Nan, Yang Li-feng, Ma Ji, Li Zhi. Bone marrow mesenchymal stem cell transplantation combined with core decompression and bone grafting in the repair of osteonecrosis of femoral head[J]. Chinese Journal of Tissue Engineering Research, 2015, 19(6): 883-890.
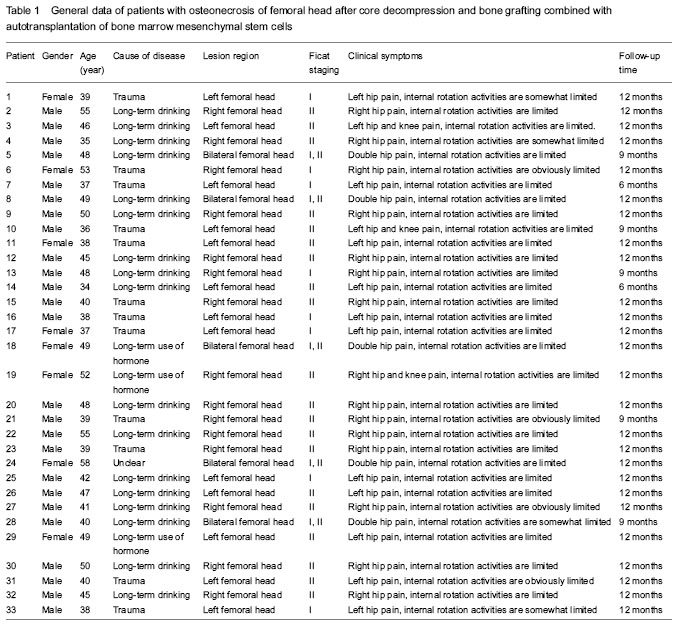
All patients were involved in the final analysis. Patients and clinical information are listed in Table 1.
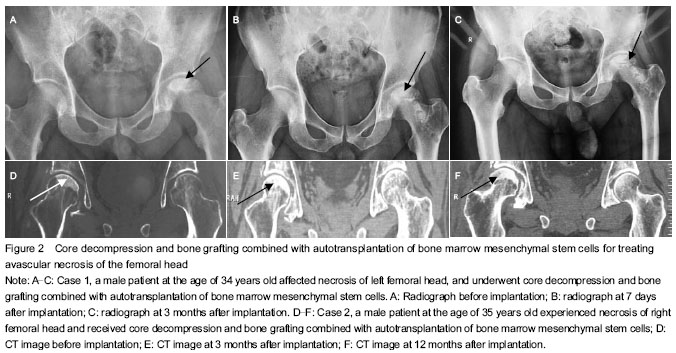
Case 1: a 34-year-old male patient suffered from necrosis of
One patient suffered from high blood pressure. One patient had joint effusion with a safety factor of 94%. Their bodies recovered to normal after corresponding treatment. Symptoms disappeared after taking corresponding measures.
| [1] Kang WL, Yuan PW. Research progress of femoral head necrosis and mesenchymal stem cells transplantation. Zhongguo Jiaoxing Waike Zazhi. 2013;21(19):1954-1957. [2] Korompilias AV, Beris AE, Lykissas MG, et al. Femoral head osteonecrosis: why choose free vascularized fibula grafting. Microsurgery. 2011;31(3):223-228. [3] Aldridge JM 3rd, Urbaniak JR. Avascular necrosis of the femoral head: etiology, pathophysiology, classification, and current treatment guidelines. Am J Orthop (Belle Mead NJ). 2004;33(7):327-332. [4] Chen C, Yang S, Feng Y, et al. Impairment of two types of circulating endothelial progenitor cells in patients with glucocorticoid-induced avascular osteonecrosis of the femoral head. Joint Bone Spine. 2013;80(1):70-76. [5] Teng M, Geng Z, Huang L, et al. Stem cell transplantation in cardiovascular disease: an update. J Int Med Res. 2012; 40(3):833-838. [6] Shen X, Wei BF. Research progress of femoral head necrosis treatment by hip-preserving surgery. Fengshibing yu Guanjieyan. 2014;3(6):68-73. [7] Fu Q, Yan SJ, Wang JY, et al. Analysis of clinical effect of core decompression combined with autologous bone-marrow mesenchymal stem cells treating 45 cases with aseptic necrosis of head of femur. Xiandai Shengwu Yixue Jinzhan. 2013;13(25):4925-4928. [8] Wang JX, Chen YZ, Wei XY. Effects of core decompression combined with transplantation of bmscs for treatment of advanced osteonecrosis of the femoral head. Zhonghua Xibao yu Ganxibao Zazhi: Dianzi Ban. 2013;3(2):83-86. [9] Katayama R, Wakitani S, Tsumaki N, et al. Repair of articular cartilage defects in rabbits using CDMP1 gene-transfected autologous mesenchymal cells derived from bone marrow. Rheumatology (Oxford). 2004;43(8):980-985. [10] Väänänen HK. Mesenchymal stem cells. Ann Med. 2005; 37(7):469-479. [11] Li ZH, Liao W, Cui XL, et al. Intravenous transplantation of allogeneic bone marrow mesenchymal stem cells and its directional migration to the necrotic femoral head. Int J Med Sci. 2011;8(1):74-83. [12] Chinese medical association. Common understanding of diagnosis and treatment for necrotic femoral heads in adults in 2012. Zhongguo Gu yu Guanjie Waike Zazhi. 2012;5(2): 185-192. [13] Li XM, Guo DH, Shi GJ, et al. Clinical study on medullary core decompression conbined with tanshinone IIA mixed with bone grafting in the treatment of osteonecrosis of the femoral head in Ficat II period. Zhongyi Zhenggu. 2014;26(5):9-12. [14] Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737-755. [15] Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Joint Surg Am. 2006;88(5):1117-1132. [16] 16 Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br. 1985; 67(1):3-9. [17] Mont MA, Ragland PS, Etienne G. Core decompression of the femoral head for osteonecrosis using percutaneous multiple small-diameter drilling. Clin Orthop Relat Res. 2004;(429): 131-138. [18] Steinberg ME, Larcom PG, Strafford B, et al. Core decompression with bone grafting for osteonecrosis of the femoral head. Clin Orthop Relat Res. 2001;(386):71-78. [19] Rijnen WH, Gardeniers JW, Buma P, et al. Treatment of femoral head osteonecrosis using bone impaction grafting. Clin Orthop Relat Res. 2003;(417):74-83. [20] Sen RK, Tripathy SK, Aggarwal S, et al. Early results of core decompression and autologous bone marrow mononuclear cells instillation in femoral head osteonecrosis: a randomized control study. J Arthroplasty. 2012;27(5):679-686. [21] Cheng JG, Yang JS. Progress in the treatment of adult avascular necrosis of femoral head. Zhongguo Xiandai Yiyao Zazhi. 2009;11(9):123-125. [22] Yang M, Li QF. The progress in the study of mesenchymal stem cells in treating ischemic injuries. Zhongguo Meirong Yixue. 2009;18(11):1709-1711. [23] Wu JQ, Cheng LM, Li ZR. Osteogenic differentiation study of bone marrow stromal stem cells in vivo. Zhongguo Gu yu Guanjie Waike. 2010;3(1):73-77. [24] Liang HS, Huang K, Li L, et al. Effect of core decompression and bone grafting combined with autotransplantation of bone marrow mesenchymal stem cells for early stage of avascular necrosis of femoral head. Zhongguo Xiandai Yiyao Zazhi. 2014;16(8):20-22. [25] Tang J, Huang K, Li L, et al. Treatment of core decompression and bone grafting combined with autotransplantation of bone marrow and platelet-rich plasma for early stage of avascular necrosis of femoral head. Yixue Lilun yu Shijian. 2013;26(10): 1273-1277. [26] Gangji V, Hauzeur JP, Matos C, et al. Treatment of osteonecrosis of the femoral head with implantation of autologous bone-marrow cells. A pilot study. J Bone Joint Surg Am. 2004;86-A(6):1153-1160. [27] Li Z, Chen G, Wang Z, et al. Treatment of avascular necrosis of the femoral head with core decompression and transplantation of autologous bone marrow mesenchymal stem cells. Zhongguo Jiaoxing Waike Zazhi. 2012;20(5): 411-414. [28] Hernigou P, Beaujean F. Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002;(405):14-23. [29] Chu JG, Wang XJ, Wang JW. Clinical curative effect of autologous bone marrow stem cell transplantation combined core decompression treatment for elderly ischemic femoral head necrosis. Zhongguo Laonian Xue Zazhi. 2012;32(16): 3432-3433. [30] Faghihi F, Baghaban Eslaminejad M. The effect of nano-scale topography on osteogenic differentiation of mesenchymal stem cells. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158(1):5-16. [31] Gentleman E, Swain RJ, Evans ND, et al. Comparative materials differences revealed in engineered bone as a function of cell-specific differentiation. Nat Mater. 2009; 8(9):763-770. [32] Chen QX. Summary of progress on the treatment of femoral head necrosis. Zhongwai Yiliao. 2014(12):197-198. [33] Cai K, Zhou YP, Wu MC. The research towards Bone marrow stem cell transplantation on femoral head necrosis. Jilin Yixue. 2013;34(2):281-282. [34] Stagg J, Galipeau J. Mechanisms of immune modulation by mesenchymal stromal cells and clinical translation. Curr Mol Med. 2013;13(5):856-867. [35] Justesen J, Stenderup K, Eriksen EF, et al. Maintenance of osteoblastic and adipocytic differentiation potential with age and osteoporosis in human marrow stromal cell cultures. Calcif Tissue Int. 2002;71(1):36-44. [36] Kang FD, Pei DX. Treatment of early necrosis of the femoral head at Ficat I, II period and before the collapse. Zhongguo Gu yu Guanjie Sunshang Zazhi. 2010;25(1):91-94. [37] Xiao YJ, Wang SR. Advance in treatment of avascular nerosis of femoral head. Zhongguo Xiandai Yisheng. 2008;46(30): 52-53. [38] Wang XX, Wu QC. Study on the surgical treatment of ischemic necrosis of femoral head. Linchuang Yixue. 2014; 34(1):119. [39] Ma YC, Liao JX, Lin Z, et al. Clinical effect of bone marrow stem cells transplantation on early avascular necrosis of femoral head. Xiandai Yiyuan. 2014;14(9):13-17. |
| [1] | 蒲 锐, 陈子扬, 袁凌燕. 不同细胞来源外泌体保护心脏的特点与效应[J]. 中国组织工程研究, 2021, 25(在线): 1-. |
| [2] | 林清凡, 解一新, 陈婉清, 叶振忠, 陈幼芳. 人胎盘源间充质干细胞条件培养液可上调缺氧状态下BeWo细胞活力和紧密连接因子的表达[J]. 中国组织工程研究, 2021, 25(在线): 4970-4975. |
| [3] | 梁 彦, 赵永飞, 徐 帅, 朱震奇, 王凯丰, 刘海鹰, 毛克亚. 影像学评估高选择性神经根封闭辅助退行性脊柱侧凸短节段固定融合的效果[J]. 中国组织工程研究, 2021, 25(9): 1423-1427. |
| [4] | 张秀梅, 翟运开, 赵 杰, 赵 萌. 类器官模型国内外数据库近10年文献研究热点分析[J]. 中国组织工程研究, 2021, 25(8): 1249-1255. |
| [5] | 李中峰, 陈明海, 凡一诺, 魏秋实, 何 伟, 陈镇秋. 右归饮治疗激素性股骨头坏死作用机制的网络药理学分析[J]. 中国组织工程研究, 2021, 25(8): 1256-1263. |
| [6] | 王正东, 黄 娜, 陈婧娴, 郑作兵, 胡鑫宇, 李 梅, 苏 晓, 苏学森, 颜 南. 丁酸钠抑制氟中毒可诱导小胶质细胞活化及炎症因子表达增多[J]. 中国组织工程研究, 2021, 25(7): 1075-1080. |
| [7] | 汪显耀, 关亚琳, 刘忠山. 提高间充质干细胞治疗难愈性创面的策略[J]. 中国组织工程研究, 2021, 25(7): 1081-1087. |
| [8] | 万 然, 史 旭, 刘京松, 王岩松. 间充质干细胞分泌组治疗脊髓损伤的研究进展[J]. 中国组织工程研究, 2021, 25(7): 1088-1095. |
| [9] | 廖成成, 安家兴, 谭张雪, 王 倩, 刘建国. 口腔鳞状细胞癌干细胞的治疗靶点及应用前景[J]. 中国组织工程研究, 2021, 25(7): 1096-1103. |
| [10] | 谢文佳, 夏天娇, 周卿云, 刘羽佳, 顾小萍. 小胶质细胞介导神经元损伤在神经退行性疾病中的作用[J]. 中国组织工程研究, 2021, 25(7): 1109-1115. |
| [11] | 李珊珊, 郭笑霄, 尤 冉, 杨秀芬, 赵 露, 陈 曦, 王艳玲. 感光细胞替代治疗视网膜变性疾病[J]. 中国组织工程研究, 2021, 25(7): 1116-1121. |
| [12] | 焦 慧, 张一宁, 宋雨晴, 林 宇, 王秀丽. 乳腺癌类器官研究进展及临床应用前景[J]. 中国组织工程研究, 2021, 25(7): 1122-1128. |
| [13] | 王诗琦, 张金生. 中医药调控缺血缺氧微环境对骨髓间充质干细胞增殖、分化及衰老的影响[J]. 中国组织工程研究, 2021, 25(7): 1129-1134. |
| [14] | 曾燕华, 郝延磊. 许旺细胞体外培养及纯化的系统性综述[J]. 中国组织工程研究, 2021, 25(7): 1135-1141. |
| [15] | 孔德胜, 何晶晶, 冯宝峰, 郭瑞云, Asiamah Ernest Amponsah, 吕 飞, 张舒涵, 张晓琳, 马 隽, 崔慧先. 间充质干细胞修复大动物模型脊髓损伤疗效评价的Meta分析[J]. 中国组织工程研究, 2021, 25(7): 1142-1148. |
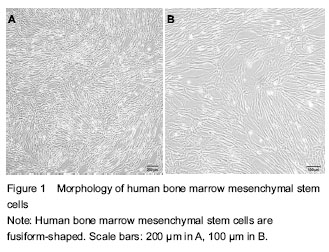
Microstructure. At present, various materials including autologous bone are used as support for filling after core decompression[7], but the therapeutic effects are poor. Currently, stem cells for treating avascular necrosis of the femoral head are a hot focus. Basic experimental researches have verified that stem cells can differentiate into osteoblasts under specific conditions, which are important factors during the repair of bone necrosis. In addition, a previous study suggested that concentrated bone marrow stem cells transplanted into the necrotic femoral head could decrease the incidence of collapse of the femoral head[8]. Bone marrow of adults consists of two kinds of cells, i.e., bone marrow hemopoietic stem cells and bone marrow mesenchymal stem cells (BMSCs). BMSCs are derived from the early developed mesoderm and ectoderm, a class of cells with multiple differentiation potentials, can differentiate into osteoblasts, chondrocytes, adipocytes, myoblasts, neurons and glial cells under certain conditions[9-10], as well as other tissues derived from mesenchymal cells. Moreover, BMSCs can be easily collected, isolated, cultured, have strong immunogenicity, weak proliferative capacity in vitro, keep the potential of multi-directional differentiation during subculture, which makes BMSCs become ideal seed cells for repair of bone necrosis[11]. To find early and give a safe effective therapy, this study used core decompression and bone grafting combined with autotransplantation of bone marrow mesenchymal stem cells for treating avascular necrosis of the femoral head, obtained apparent therapeutic effects. Reports on 33 patients with complete follow-up data and 33 hips are as follows:
Data were analyzed using SPSS 18.0 software and expressed as mean ± SD. Paired t-test was used. Harris hip joint function score was statistically analyzed before transplantation and during final follow-up. A value of P < 0.05 was considered statistically significant.
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||