[1] WILKINSON HN, HARDMAN MJ. Wound healing: cellular mechanisms and pathological outcomes. Open Biol. 2020;10(9):200223.
[2] LEGRAND JMD, MARTINO MM. Growth Factor and Cytokine Delivery Systems for Wound Healing. Cold Spring Harb Perspect Biol. 2022;14(8):a041234.
[3] YAMAKAWA S, HAYASHIDA K. Advances in surgical applications of growth factors for wound healing. Burns Trauma. 2019;7:10.
[4] NIU Y, LI Q, DING Y, et al. Engineered delivery strategies for enhanced control of growth factor activities in wound healing. Adv Drug Deliv Rev. 2019;146:190-208.
[5] EVERTS P, OOISHI K, JAYARAM P, et al. Platelet-Rich Plasma: New Performance Understandings and Therapeutic Considerations in 2020. Int J Mol Sci. 2020;21(20):7794.
[6] VERMA R, KUMAR S, GARG P, et al. Platelet-rich plasma: a comparative and economical therapy for wound healing and tissue regeneration. Cell Tissue Bank. 2022;12:1-22.
[7] 刘宗星,江丽,邹细平,等.自体富血小板凝胶促进创面愈合的临床研究[J].当代医学,2022,28(4):61-64.
[8] GODOI TTF, RODRIGUES BL, HUBER SC, et al. Platelet-Rich Plasma Gel Matrix (PRP-GM): Description of a New Technique. Bioengineering (Basel). 2022;9(12):817.
[9] ONETO P, ETULAIN J. PRP in wound healing applications. Platelets. 2021;32(2):189-199.
[10] ATTILI AR, IACOUCCI C, SERRI E, et al. Antibacterial Properties of Canine Platelet-Rich Plasma and Other Non-Transfusional Hemo-Components: An in vitro Study. Front Vet Sci. 2021;8:746809.
[11] SCHAR MO, DIAZ-ROMERO J, KOHL S, et al. Platelet-rich concentrates differentially release growth factors and induce cell migration in vitro. Clin Orthop Relat Res. 2015;473(5):1635-1643.
[12] DOHAN EHRENFEST DM, RASMUSSON L, ALBREKTSSON T. Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends Biotechnol. 2009; 27(3):158-167.
[13] EMING SA, MARTIN P, TOMIC-CANIC M. Wound repair and regeneration: mechanisms, signaling, and translation. Sci Transl Med. 2014;6(265):265sr6.
[14] VASILE C, PAMFIL D, STOLERU E, et al. New Developments in Medical Applications of Hybrid Hydrogels Containing Natural Polymers. Molecules. 2020;25(7):1539.
[15] HU H, XU FJ. Rational design and latest advances of polysaccharide-based hydrogels for wound healing. Biomater Sci. 2020;8(8):2084-2101.
[16] ZHAO W, LI Y, ZHANG X, et al. Photo-responsive supramolecular hyaluronic acid hydrogels for accelerated wound healing. J Control Release. 2020;323:24-35.
[17] LIU C, MA Y, GUO S, et al. Topical delivery of chemotherapeutic drugs using nano-hybrid hydrogels to inhibit post-surgical tumour recurrence. Biomater Sci. 2021;9(12):4356-4363.
[18] PAN Q, FAN R, CHEN R, et al. Weakly acidic microenvironment of the wound bed boosting the efficacy of acidic fibroblast growth factor to promote skin regeneration. Front Bioeng Biotechnol. 2023;11:1150819.
[19] BAHADORAN M, SHAMLOO A, NOKOORANI YD. Development of a polyvinyl alcohol/sodium alginate hydrogel-based scaffold incorporating bFGF-encapsulated microspheres for accelerated wound healing. Sci Rep. 2020;10(1):7342.
[20] KUTLU B, TIGLI AYDIN RS, AKMAN AC, et al. Platelet-rich plasma-loaded chitosan scaffolds: preparation and growth factor release kinetics. J Biomed Mater Res B Appl Biomater. 2013;101(1):28-35.
[21] SON SR, SARKAR SK, NGUYEN-THUY BL, et al. Platelet-rich plasma encapsulation in hyaluronic acid/gelatin-BCP hydrogel for growth factor delivery in BCP sponge scaffold for bone regeneration. J Biomater Appl. 2015;29(7):988-1002.
[22] GROWNEY EA, LINDER HR, GARG K, et al. Bio-conjugation of platelet-rich plasma and alginate through carbodiimide chemistry for injectable hydrogel therapies. J Biomed Mater Res B Appl Biomater. 2020;108(5):1972-1984.
[23] CENSI R, CASADIDIO C, DENG S, et al. Interpenetrating Hydrogel Networks Enhance Mechanical Stability, Rheological Properties, Release Behavior and Adhesiveness of Platelet-Rich Plasma. Int J Mol Sci. 2020;21(4):1399.
[24] JAIN E, SHETH S, DUNN A, et al. Sustained release of multicomponent platelet-rich plasma proteins from hydrolytically degradable PEG hydrogels. J Biomed Mater Res A. 2017;105(12):3304-3314.
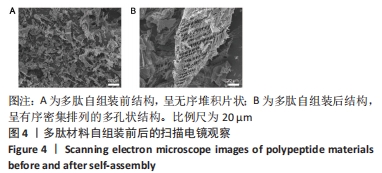
[25] 谭婷媛.多肽超分子网络的构建及凝胶性能调控[D].北京:中国科学院大学(中国科学院上海应用物理研究所),2022.
[26] 王韵晴,卢婷利,陈婷,等.自组装多肽支架材料的研究进展[J].材料科学与工程学报,2012,30(2):324-328+311.
[27] 元亮亮,梁鹏.自组装多肽纳米纤维支架的结构特点及应用优势[J].中国组织工程研究,2013,17(29):5379-5386.
[28] LI J, WANG L, YI X, et al. Platelet 3D preservation using a novel biomimetic nanofiber peptide for reduced apoptosis and easy storage. ACS Appl Mater Interfaces. 2021;13(32):38040-38049.
[29] 李佳瑶.生物纳米材料在血小板包装储运中的应用研究[D].天津:天津科技大学,2021.
[30] WANG P, BERRY D, MORAN A, et al. Controlled growth factor release in 3D-printed hydrogels. Adv Healthc Mater. 2020;9(15):e1900977.
[31] ULIJN RV, SMITH AM. Designing peptide based nanomaterials. Chem Soc Rev. 2008;37(4):664-675.
[32] KIM HS, SUN X, LEE JH, et al. Advanced drug delivery systems and artificial skin grafts for skin wound healing. Adv Drug Deliv Rev. 2019; 146:209-239.
[33] ZHAO X, WU H, GUO B, et al. Antibacterial anti-oxidant electroactive injectable hydrogel as self-healing wound dressing with hemostasis and adhesiveness for cutaneous wound healing. Biomaterials. 2017;122: 34-47.
[34] KEIL C, HUBNER C, RICHTER C, et al. Ca-Zn-Ag Alginate Aerogels for Wound Healing Applications: Swelling Behavior in Simulated Human Body Fluids and Effect on Macrophages. Polymers (Basel). 2020; 12(11):2741.
[35] ZHENG Z, LI M, SHI P, et al. Polydopamine-modified collagen sponge scaffold as a novel dermal regeneration template with sustained release of platelet-rich plasma to accelerate skin repair: A one-step strategy. Bioact Mater. 2021;6(8):2613-2628.
[36] QIU M, CHEN D, SHEN C, et al. Platelet-rich plasma-loaded poly(D,L-lactide)-poly(ethylene glycol)-poly(D,L-lactide) hydrogel dressing promotes full-thickness skin wound healing in a rodent model. Int J Mol Sci. 2016;17(7):1001.
[37] CHEN J, ZOU X. Self-assemble peptide biomaterials and their biomedical applications. Bioact Mater. 2019;4:120-131.
[38] CALVELO M, GRANJA JR, GARCIA-FANDINO R. Competitive double-switched self-assembled cyclic peptide nanotubes: a dual internal and external control. Phys Chem Chem Phys. 2019;21(37):20750-20756.
[39] CAO M, WANG Y, HU X, et al. Reversible thermoresponsive peptide-PNIPAM hydrogels for controlled drug delivery. Biomacromolecule. 2019;20(9):3601-3610.
[40] El BACKLY RM, ZAKY SH, MURAGLIA A, et al. A platelet-rich plasma-based membrane as a periosteal substitute with enhanced osteogenic and angiogenic properties: a new concept for bone repair. Tissue Eng Part A. 2013;19(1-2):152-165.
[41] ROSADI I, KARINA K, ROSLIANA I, et al. In vitro study of cartilage tissue engineering using human adipose-derived stem cells induced by platelet-rich plasma and cultured on silk fibroin scaffold. Stem Cell Res Ther. 2019;10(1):369.
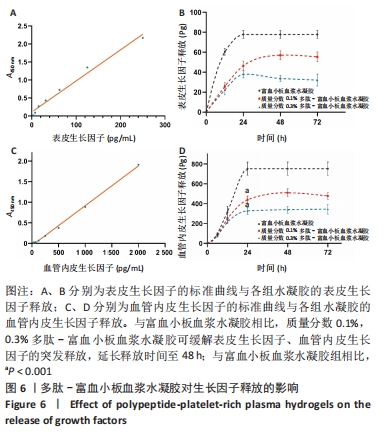
[42] YANG HS, SHIN J, BHANG SH, et al. Enhanced skin wound healing by a sustained release of growth factors contained in platelet-rich plasma. Exp Mol Med. 2011;43(11):622-629.
[43] TAMBELLA AM, ATTILI AR, DUPRE G, et al. Del Fabbro M. Platelet-rich plasma to treat experimentally-induced skin wounds in animals: A systematic review and meta-analysis. PLoS One. 2018;13(1):e0191093.
[44] CHOI SM, LEE KM, KIM HJ, et al. Effects of structurally stabilized EGF and bFGF on wound healing in type I and type II diabetic mice. Acta Biomater. 2018;66:325-334.
[45] APTE RS, CHEN DS, FERRARA N. VEGF in signaling and disease: beyond discovery and development. Cell. 2019;176(6):1248-1264.
[46] MARTINO MM, BRIQUEZ PS, RANGA A, et al. Heparin-binding domain of fibrin(ogen) binds growth factors and promotes tissue repair when incorporated within a synthetic matrix. Proc Natl Acad Sci U S A. 2013; 110(12):4563-4568. |