[1] RAVINDRA VM, SENGLAUB SS, RATTANI A, et al. Degenerative lumbar spine disease: estimating global incidence and worldwide volume. Global Spine J. 2018;8(8):784-794.
[2] MOBBS RJ, PHAN K, MALHAM G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015; 1(1):2-18.
[3] LEE CK, LANGRANA NA. A review of spinal fusion for degenerative disc disease: need for alternative treatment approach of disc arthroplasty? Spine J. 2004;4(6 Suppl):173s-176s.
[4] HERRERA A, YÁNEZ A, MARTEL O, et al. Computational study and experimental validation of porous structures fabricated by electron beam melting: a challenge to avoid stress shielding. Mater Sci Eng C Mater Biol Appl. 2014;45:89-93.
[5] AGARWAL R, WILLIAMS K, UMSCHEID CA, et al. Osteoinductive bone graft substitutes for lumbar fusion: a systematic review. J Neurosurg Spine. 2009;11(6):729-740.
[6] KAISER MG, GROFF MW, WATTERS WC, 3RD, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 16: bone graft extenders and substitutes as an adjunct for lumbar fusion. J Neurosurg Spine. 2014;21(1):106-132.
[7] ZOU D, JIANG S, ZHOU S, et al. Prevalence of osteoporosis in patients undergoing lumbar fusion for lumbar degenerative diseases: a combination of dxa and hounsfield units. Spine (Phila Pa 1976). 2020; 45(7):E406-E410.
[8] ALPANTAKI K, KAMPOUROGLOU A, KOUTSERIMPAS C, et al. Diabetes mellitus as a risk factor for intervertebral disc degeneration: a critical review. Eur Spine J. 2019;28(9):2129-2144.
[9] GUZMAN JZ, IATRIDIS JC, SKOVRLJ B, et al. Outcomes and complications of diabetes mellitus on patients undergoing degenerative lumbar spine surgery. Spine (Phila Pa 1976). 2014;39(19):1596-1604.
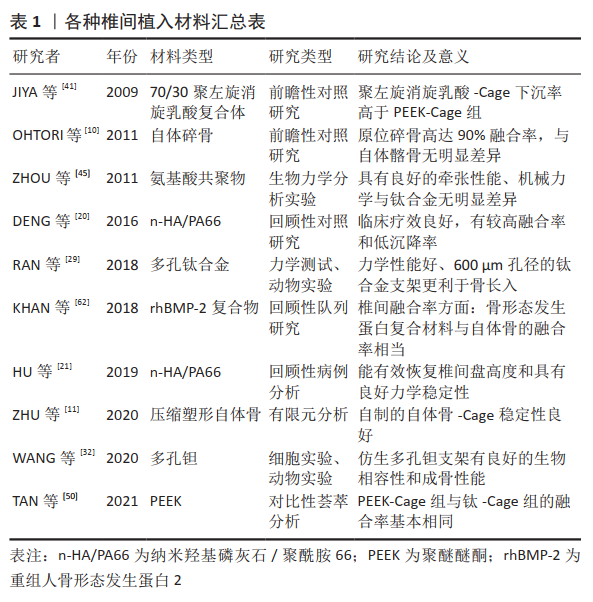
[10] OHTORI S, SUZUKI M, KOSHI T, et al. Single-level instrumented posterolateral fusion of the lumbar spine with a local bone graft versus an iliac crest bone graft: a prospective, randomized study with a 2-year follow-up. Eur Spine J. 2011;20(4):635-639.
[11] ZHU H, ZHONG W, ZHANG P, et al. Biomechanical evaluation of autologous bone-cage in posterior lumbar interbody fusion: a finite element analysis. BMC Musculoskelet Disord. 2020;21(1):379.
[12] KOEHLER S, HELD C, STETTER C, et al. Alloplastic or autologous? Bone chips versus peek cage for lumbar interbody fusion in degenerative spondylolisthesis. J Neurol Surg A Cent Eur Neurosurg. 2021. doi:10.1055/s-0040-1718770.
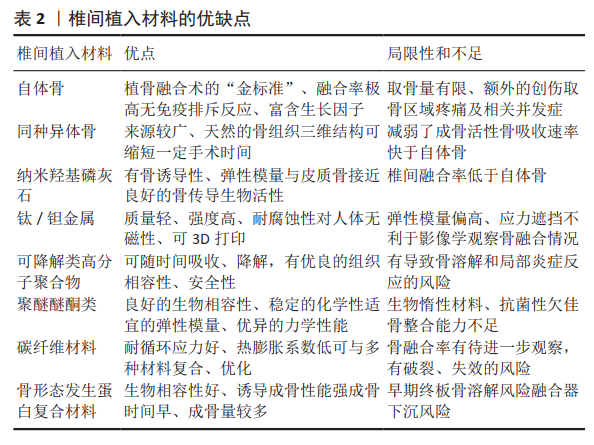
[13] Ehrler DM, Vaccaro AR. The use of allograft bone in lumbar spine surgery. Clin Orthop Relat Res. 2000;(371):38-45.
[14] GARCÍA DE FRUTOS A, GONZÁLEZ-TARTIÈRE P, COLL BONET R, et al. Randomized clinical trial: expanded autologous bone marrow mesenchymal cells combined with allogeneic bone tissue, compared with autologous iliac crest graft in lumbar fusion surgery. Spine J. 2020; 20(12):1899-1910.
[15] BUSER Z, BRODKE DS, YOUSSEF JA, et al. Synthetic bone graft versus autograft or allograft for spinal fusion: a systematic review. J Neurosurg Spine. 2016;25(4):509-516.
[16] HIROSHI Y. Heterotopic bone formation around porous hydroxyapatite ceramics in the subcutis of dogs. J Oral Biosci. 1990;32(2):190-192.
[17] RIPAMONTI U. The morphogenesis of bone in replicas of porous hydroxyapatite obtained from conversion of calcium carbonate exoskeletons of coral. J Bone Joint Surg Am. 1991;73(5):692-703.
[18] ZHANG L, HANAGATA N, MAEDA M, et al. Porous hydroxyapatite and biphasic calcium phosphate ceramics promote ectopic osteoblast differentiation from mesenchymal stem cells. Sci Technol Adv Mater. 2009;10(2):025003.
[19] DAVISON NL, SU J, YUAN H, et al. Influence of surface microstructure and chemistry on osteoinduction and osteoclastogenesis by biphasic calcium phosphate discs. Eur Cell Mater. 2015;29:314-329.
[20] DENG QX, OU YS, ZHU Y, et al. Clinical outcomes of two types of cages used in transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases: n-HA/PA66 cages versus PEEK cages. J Mater Sci Mater Med. 2016;27(6):102.
[21] HU J, OU Y, ZHU Y, et al. Effectiveness of nano-hydroxyapatite/polyamide-66 Cage in interbody fusion for degenerative lumbar scoliosis. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33(3):287-295.
[22] KUSHIOKA J, KAITO T, MAKINO T, et al. Difference in the fusion rate and bone formation between artificial bone and iliac autograft inside an inter-body fusion cage - A comparison between porous hydroxyapatite/type 1 collagen composite and autologous iliac bone. J Orthop Sci. 2018;23(4):622-626.
[23] MCGILVRAY KC, EASLEY J, SEIM HB, et al. Bony ingrowth potential of 3D-printed porous titanium alloy: a direct comparison of interbody cage materials in an in vivo ovine lumbar fusion model. Spine J. 2018; 18(7):1250-1260.
[24] VLAD MD, FERNÁNDEZ AGUADO E, GÓMEZ GONZÁLEZ S, et al. Novel titanium-apatite hybrid scaffolds with spongy bone-like micro architecture intended for spinal application: in vitro and in vivo study. Mater Sci Eng C Mater Biol Appl. 2020;110:110658.
[25] ICHIOKA Y, ASA’AD F, MALEKZADEH B, et al. Epigenetic changes of osteoblasts in response to titanium surface characteristics. J Biomed Mater Res A. 2021;109(2):170-180.
[26] LOTZ EM, BERGER MB, SCHWARTZ Z, et al. Regulation of osteoclasts by osteoblast lineage cells depends on titanium implant surface properties. Acta Biomater. 2018;68:296-307.
[27] ZHENG Y, HAN Q, WANG J, et al. Promotion of osseointegration between implant and bone interface by titanium alloy porous scaffolds prepared by 3D printing. ACS Biomater Sci Eng. 2020;6(9):5181-5190.
[28] PENG WM, LIU YF, JIANG XF, et al. Bionic mechanical design and 3D printing of novel porous Ti6Al4V implants for biomedical applications. J Zhejiang Univ Sci B. 2019;20(8):647-659.
[29] RAN Q, YANG W, HU Y, et al. Osteogenesis of 3D printed porous Ti6Al4V implants with different pore sizes. J Mech Behav Biomed Mater. 2018; 84:1-11.
[30] LU M, XU S, LEI ZX, et al. Application of a novel porous tantalum implant in rabbit anterior lumbar spine fusion model: in vitro and in vivo experiments. Chin Med J (Engl). 2019;132(1):51-62.
[31] PATEL MS, MCCORMICK JR, GHASEM A, et al. Tantalum: the next biomaterial in spine surgery? J Spine Surg. 2020;6(1):72-86.
[32] WANG X, ZHU Z, XIAO H, et al. Three-dimensional, multiscale, and interconnected trabecular bone mimic porous tantalum scaffold for bone tissue engineering. ACS Omega. 2020;5(35):22520-22528.
[33] WANG Q, ZHANG H, LI Q, et al. Biocompatibility and osteogenic properties of porous tantalum. Exp Ther Med. 2015;9(3):780-786.
[34] MATEJKA J, ZEMAN J, BELATKA J. Mid-term results of 360-degree lumbar spondylodesis with the use of a tantalum implant for disc replacement. Acta Chir Orthop Traumatol Cech. 2009;76(5):388-393.
[35] LEQUIN MB, VERBAAN D, BOUMA GJ. Posterior lumbar interbody fusion with stand-alone Trabecular Metal cages for repeatedly recurrent lumbar disc herniation and back pain. J Neurosurg Spine. 2014;20(6):617-622.
[36] HOJO Y, KOTANI Y, ITO M, et al. A biomechanical and histological evaluation of a bioresorbable lumbar interbody fusion cage. Biomaterials. 2005;26(15):2643-2651.
[37] LOWE TG, COE JD. Resorbable polymer implants in unilateral transforaminal lumbar interbody fusion. J Neurosurg. 2002;97(4 Suppl): 464-467.
[38] MAIA-PINTO MOC, BROCHADO ACB, TEIXEIRA BN, et al. Biomimetic mineralization on 3D printed pla scaffolds: on the response of human primary osteoblasts spheroids and in vivo implantation. Polymers (Basel). 2020. doi:10.3390/polym13010074.
[39] HAN SH, CHA M, JIN YZ, et al. BMP-2 and hMSC dual delivery onto 3D printed PLA-Biogel scaffold for critical-size bone defect regeneration in rabbit tibia. Biomed Mater. 2020;16(1):015019.
[40] COUTURE DE, BRANCH CL JR. Posterior lumbar interbody fusion with bioabsorbable spacers and local autograft in a series of 27 patients. Neurosurg Focus. 2004;16(3):E8.
[41] JIYA T, SMIT T, DEDDENS J, et al. Posterior lumbar interbody fusion using nonresorbable poly-ether-ether-ketone versus resorbable poly-L-lactide-co-D, L-lactide fusion devices: a prospective, randomized study to assess fusion and clinical outcome. Spine (Phila Pa 1976). 2009; 34(3):233-237.
[42] FROST A, BAGOURI E, BROWN M, et al. Osteolysis following resorbable poly-L-lactide-co-D, L-lactide PLIF cage use: a review of cases. Eur Spine J. 2012;21(3):449-454.
[43] 邵洪波.新型氨基酸共聚物/磷酸钙复合骨修复材料的相关研究[D].石家庄:河北医科大学,2015.
[44] REN C, SONG Y, XUE Y, et al. Evaluation of bioabsorbable multiamino acid copolymer/nanohydroxyapatite/calcium sulfate cage in a goat spine model. World Neurosurg. 2017;103:341-347.
[45] CHUNGUANG Z, YUEMING S, CHONGQI T, et al. Evaluation of bioabsorbable multiamino acid copolymer/α-tri-calcium phosphate interbody fusion cages in a goat model. Spine (Phila Pa 1976). 2011; 36(25):E1615-E1622.
[46] 毛誉蓉,孙佳敏,周雄,等.医用特种高分子聚醚醚酮植入体及其表面界面工程[J].功能高分子学报,2021,34(2):144-160.
[47] KURTZ SM, DEVINE JN. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials. 2007;28(32):4845-4869.
[48] SÉNÉGAS J. Mechanical supplementation by non-rigid fixation in degenerative intervertebral lumbar segments: the Wallis system. Eur Spine J. 2002;11 Suppl 2(Suppl 2):S164-S169.
[49] YAO YC, CHOU PH, LIN HH, et al. Outcome of Ti/PEEK Versus PEEK cages in minimally invasive transforaminal lumbar interbody fusion. Global Spine J. 2021. doi:10.1177/21925682211000323.
[50] TAN JH, CHEONG CK, HEY HWD. Titanium (Ti) cages may be superior to polyetheretherketone (PEEK) cages in lumbar interbody fusion: a systematic review and meta-analysis of clinical and radiological outcomes of spinal interbody fusions using Ti versus PEEK cages. Eur Spine J. 2021. doi:10.1007/s00586-021-06748-w.
[51] KASHII M, KITAGUCHI K, MAKINO T, et al. Comparison in the same intervertebral space between titanium-coated and uncoated PEEK cages in lumbar interbody fusion surgery. J Orthop Sci. 2020;25(4): 565-570.
[52] WANG S, DENG Y, YANG L, et al. Enhanced antibacterial property and osteo-differentiation activity on plasma treated porous polyetheretherketone with hierarchical micro/nano-topography. J Biomater Sci Polym Ed. 2018;29(5):520-542.
[53] XUE Z, WANG Z, SUN A, et al. Rapid construction of polyetheretherketone (PEEK) biological implants incorporated with brushite (CaHPO(4)·2H(2)O) and antibiotics for anti-infection and enhanced osseointegration. Mater Sci Eng C Mater Biol Appl. 2020; 111:110782.
[54] BRANTIGAN JW, STEFFEE AD, GEIGER JM. A carbon fiber implant to aid interbody lumbar fusion. Mechanical testing. Spine (Phila Pa 1976). 1991;16(6 Suppl):S277-S282.
[55] 宋成哲,金红旭.碳纤维椎间融合器与钛网椎间融合器修复腰椎退行性变:生物相容性比较[J].中国组织工程研究,2015,19(12): 1909-1913.
[56] BONNHEIM N, ANSARI F, REGIS M, et al. Effect of carbon fiber type on monotonic and fatigue properties of orthopedic grade PEEK. J Mech Behav Biomed Mater. 2019;90:484-492.
[57] HEARY RF, PARVATHREDDY NK, QAYUMI ZS, et al. Suitability of carbon fiber-reinforced polyetheretherketone cages for use as anterior struts following corpectomy. J Neurosurg Spine. 2016;25(2):248-255.
[58] 王二平,朱姝,谭宗尚,等.CF/PEEK复合材料的性能研究[J].纤维复合材料,2020,37(4):35-38.
[59] SARDAR Z, JARZEM P. Failure of a carbon fiber-reinforced polymer implant used for transforaminal lumbar interbody fusion. Global Spine J. 2013;3(4):253-256.
[60] NOURIAN AA, HARRINGTON J, PULIDO PA, et al. Fusion rates of lateral lumbar interbody fusion using recombinant human bone morphogenetic protein-2. Global Spine J. 2019;9(4):398-402.
[61] VINCENTELLI AF, SZADKOWSKI M, VARDON D, et al. rhBMP-2 (Recombinant Human Bone Morphogenetic Protein-2) in real world spine surgery. A phase IV, National, multicentre, retrospective study collecting data from patient medical files in French spinal centres. Orthop Traumatol Surg Res. 2019;105(6):1157-1163.
[62] KHAN TR, PEARCE KR, MCANANY SJ, et al. Comparison of transforaminal lumbar interbody fusion outcomes in patients receiving rhBMP-2 versus autograft. Spine J. 2018;18(3):439-446.
[63] 翁汭,叶林强,黄学成,等.重组人骨形态发生蛋白2联合自体骨行椎间植骨融合治疗胸腰椎结核[J].中国组织工程研究,2020, 24(23):3609-3614.
[64] LYTLE EJ, LAWLESS MH, PAIK G, et al. The minimally effective dose of bone morphogenetic protein in posterior lumbar interbody fusion: a systematic review and meta-analysis. Spine J. 2020;20(8):1286-1304.
[65] LI Z, WANG S, XU G, et al. Synergy effect of Sr and rhBMP-2: a potential solution to osteolysis caused by rhBMP-2. Med Hypotheses. 2020;144:109895.
[66] ROSEN CD, KIESTER PD, LEE TQ. Pseudo-pedicle heterotopic ossification from use of recombinant human bone morphogenetic protein 2 (rhBMP-2) in transforaminal lumbar interbody fusion cages. Am J Orthop (Belle Mead NJ). 2018. doi:10.12788/ajo.2018.0003. |
 文题释义:
文题释义: