[1] BAIGUERA S, RIBATTI D. Endothelialization approaches for viable engineered tissues. Angiogenesis. 2013;16(1):1-14.
[2] MASSON-MEYERS DS, TAYEBI L. Vascularization strategies in tissue engineering approaches for soft tissue repair. J Tissue Eng Regen Med. 2021;15(9):747-762.
[3] LASCHKE MW, MENGER MD. The simpler, the better: tissue vascularization using the body’s own resources. Trends Biotechnol. 2022;40(3):281-290.
[4] ZUK PA, ZHU M, MIZUNO H, et al. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001;7(2):211-228.
[5] GURTNER GC, WERNER S, BARRANDON Y, et al. Wound repair and regeneration. Nature. 2008;453(7193):314-321.
[6] FINNSON KW, MCLEAN S, DI GUGLIELMO GM, et al.Dynamics of Transforming Growth Factor Beta Signaling in Wound Healing and Scarring. Adv Wound Care (New Rochelle). 2013;2(5):195-214.
[7] DIPIETRO LA. Angiogenesis and wound repair: when enough is enough. J Leukoc Biol. 2016;100(5):979-984.
[8] VEITH AP, HENDERSON K, SPENCER A, et al. Therapeutic strategies for enhancing angiogenesis in wound healing. Adv Drug Deliv Rev. 2019;146: 97-125.
[9] AHLUWALIA A, TARNAWSKI AS. Critical role of hypoxia sensor--HIF-1alpha in VEGF gene activation. Implications for angiogenesis and tissue injury healing. Curr Med Chem. 2012;19(1):90-97.
[10] WIETECHA MS, KROL MJ, MICHALCZYK ER, et al. Pigment epithelium-derived factor as a multifunctional regulator of wound healing. Am J Physiol Heart Circ Physiol. 2015;309(5):H812-H826.
[11] WIETECHA MS, CHEN L, RANZER MJ, et al. Sprouty2 downregulates angiogenesis during mouse skin wound healing. Am J Physiol Heart Circ Physiol. 2011;300(2):H459-H467.
[12] HAKANPAA L, SIPILA T, LEPPANEN VM, et al. Endothelial destabilization by angiopoietin-2 via integrin beta1 activation. Nat Commun. 2015;6:5962.
[13] SESE B, SANMARTIN JM, ORTEGA B, et al. Nanofat Cell Aggregates: A Nearly Constitutive Stromal Cell Inoculum for Regenerative Site-Specific Therapies. Plast Reconstr Surg. 2019;144(5):1079-1088.
[14] LANGE-ASSCHENFELDT B, VELASCO P, STREIT M, et al. The angiogenesis inhibitor vasostatin does not impair wound healing at tumor-inhibiting doses. J Invest Dermatol. 2001;117(5):1036-1041.
[15] WILGUS TA, FERREIRA AM, OBERYSZYN TM, et al. Regulation of scar formation by vascular endothelial growth factor. Lab Invest. 2008;88(6): 579-590.
[16] ERBA P, OGAWA R, ACKERMANN M, et al. Angiogenesis in wounds treated by microdeformational wound therapy. Ann Surg. 2011;253(2):402-409.
[17] DATTA P, AYAN B, OZBOLAT IT. Bioprinting for vascular and vascularized tissue biofabrication. Acta Biomater. 2017;51:1-20.
[18] MIN S, KO IK, YOO JJ. State-of-the-Art Strategies for the Vascularization of Three-Dimensional Engineered Organs. Vasc Specialist Int. 2019;35(2):77-89.
[19] COPCU HE, OZTAN S. Not Stromal Vascular Fraction (SVF) or Nanofat, but Total Stromal-Cells (TOST): A New Definition. Systemic Review of Mechanical Stromal-Cell Extraction Techniques. Tissue Eng Regen Med. 2021;18(1):25-36.
[20] ALEXANDER RW. Biocellular Regenerative Medicine: Use of Adipose-Derived Stem/Stromal Cells and It’s Native Bioactive Matrix. Phys Med Rehabil Clin N Am. 2016;27(4):871-891.
[21] COHEN SR, HEWETT S, ROSS L, et al. Regenerative Cells For Facial Surgery: Biofilling and Biocontouring. Aesthet Surg J. 2017;37(suppl_3):S16-S32.
[22] BORA P, MAJUMDAR AS. Adipose tissue-derived stromal vascular fraction in regenerative medicine: a brief review on biology and translation. Stem Cell Res Ther. 2017;8(1):145.
[23] FRUEH FS, MENGER MD, LINDENBLATT N, et al. Current and emerging vascularization strategies in skin tissue engineering. Crit Rev Biotechnol. 2017;37(5):613-625.
[24] SUN Y, CHEN S, ZHANG X, et al. Significance of Cellular Cross-Talk in Stromal Vascular Fraction of Adipose Tissue in Neovascularization. Arterioscler Thromb Vasc Biol. 2019;39(6):1034-1044.
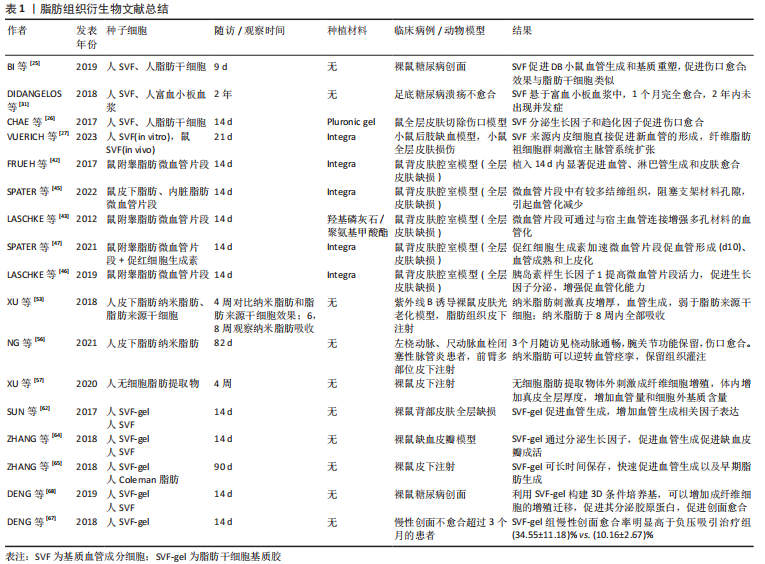
[25] BI H, LI H, ZHANG C, et al. Stromal vascular fraction promotes migration of fibroblasts and angiogenesis through regulation of extracellular matrix in the skin wound healing process. Stem Cell Res Ther. 2019;10(1):302.
[26] CHAE DS, HAN S, SON M, et al. Stromal vascular fraction shows robust wound healing through high chemotactic and epithelialization property. Cytotherapy. 2017;19(4):543-554.
[27] VUERICH R, GROPPA E, VODRET S, et al. Ischemic wound revascularization by the stromal vascular fraction relies on host-donor hybrid vessels. NPJ Regen Med. 2023;8(1):8.
[28] 朱琳,李薇薇,刘志凯.人血管基质片段联合脂肪干细胞促进裸鼠放射性皮肤损伤的愈合[J]. 山东大学学报(医学版),2017,55(9):66-72.
[29] STACHURA A, PASKAL W, PAWLIK W, et al. The Use of Adipose-Derived Stem Cells (ADSCs) and Stromal Vascular Fraction (SVF) in Skin Scar Treatment-A Systematic Review of Clinical Studies. J Clin Med. 2021;10(16):3637.
[30] ZHAO X, GUO J, ZHANG F, et al. Therapeutic application of adipose-derived stromal vascular fraction in diabetic foot. Stem Cell Res Ther. 2020; 11(1):394.
[31] DIDANGELOS T, KOLIAKOS G, KOUZI K, et al. Accelerated healing of a diabetic foot ulcer using autologous stromal vascular fraction suspended in platelet-rich plasma. Regen Med. 2018;13(3):277-281.
[32] TAN SS, YEO XY, LIANG ZC, et al. Stromal vascular fraction promotes fibroblast migration and cellular viability in a hyperglycemic microenvironment through up-regulation of wound healing cytokines. Exp Mol Pathol. 2018;104(3):250-255.
[33] ROATO I, BELISARIO DC, COMPAGNO M, et al. Adipose-Derived Stromal Vascular Fraction/Xenohybrid Bone Scaffold: An Alternative Source for Bone Regeneration. Stem Cells Int. 2018;2018:4126379.
[34] KAMENAGA T, KURODA Y, NAGAI K, et al. Cryopreserved human adipose-derived stromal vascular fraction maintains fracture healing potential via angiogenesis and osteogenesis in an immunodeficient rat model. Stem Cell Res Ther. 2021;12(1):110.
[35] MAZO M, CEMBORAIN A, GAVIRA JJ, et al. Adipose stromal vascular fraction improves cardiac function in chronic myocardial infarction through differentiation and paracrine activity. Cell Transplant. 2012;21(5):1023-1037.
[36] 袁艺, 鲁峰, 高建华. 血管基质片段辅助游离脂肪移植早期移植物组织学变化及相关实验研究[J]. 中国修复重建外科杂志,2013,27(4):449-453.
[37] RAMAKRISHNAN VM, BOYD NL. The Adipose Stromal Vascular Fraction as a Complex Cellular Source for Tissue Engineering Applications. Tissue Eng Part B Rev. 2018;24(4):289-299.
[38] 鲁峰, 常强, 詹炜卿, 等. 血管基质片段促进体内组织工程室血管和组织新生的初步研究[J]. 中国修复重建外科杂志,2014,28(5):644-648.
[39] FRANCOIS P, GIRAUDO L, VERAN J, et al. Development and Validation of a Fully GMP-Compliant Process for Manufacturing Stromal Vascular Fraction: A Cost-Effective Alternative to Automated Methods. Cells. 2020;9(10):2158.
[40] FRUEH FS, SPATER T, SCHEUER C, et al. Isolation of Murine Adipose Tissue-derived Microvascular Fragments as Vascularization Units for Tissue Engineering. J Vis Exp. 2017;(122):55721.
[41] LASCHKE MW, SPATER T, MENGER MD. Microvascular Fragments: More Than Just Natural Vascularization Units. Trends Biotechnol. 2021;39(1):24-33.
[42] FRUEH FS, SPATER T, LINDENBLATT N, et al. Adipose Tissue-Derived Microvascular Fragments Improve Vascularization, Lymphangiogenesis, and Integration of Dermal Skin Substitutes. J Invest Dermatol. 2017;137(1):217-227.
[43] LASCHKE MW, KLEER S, SCHEUER C, et al. Vascularisation of porous scaffolds is improved by incorporation of adipose tissue-derived microvascular fragments. Eur Cell Mater. 2012;24:266-277.
[44] ORTH M, ALTMEYER MAB, SCHEUER C, et al. Effects of locally applied adipose tissue-derived microvascular fragments by thermoresponsive hydrogel on bone healing. Acta Biomater. 2018;77:201-211.
[45] SPATER T, MARSCHALL JE, BRUCKER LK, et al. Vascularization of Microvascular Fragment Isolates from Visceral and Subcutaneous Adipose Tissue of Mice. Tissue Eng Regen Med. 2022;19(1):161-175.
[46] LASCHKE MW, KONTAXI E, SCHEUER C, et al. Insulin-like growth factor 1 stimulates the angiogenic activity of adipose tissue-derived microvascular fragments. J Tissue Eng. 2019;10:2041731419879837.
[47] SPATER T, WORRINGER DM, MENGER MM, et al. Systemic low-dose erythropoietin administration improves the vascularization of collagen-glycosaminoglycan matrices seeded with adipose tissue-derived microvascular fragments. J Tissue Eng. 2021;12:20417314211000304.
[48] XU X, LIANG C, GAO X, et al. Adipose Tissue-derived Microvascular Fragments as Vascularization Units for Dental Pulp Regeneration. J Endod. 2021;47(7):1092-1100.
[49] TONNARD P, VERPAELE A, PEETERS G, et al. Nanofat grafting: basic research and clinical applications. Plast Reconstr Surg. 2013;132(4):1017-1026.
[50] KAMAT P, FRUEH FS, MCLUCKIE M, et al. Adipose tissue and the vascularization of biomaterials: Stem cells, microvascular fragments and nanofat-a review. Cytotherapy. 2020;22(8):400-411.
[51] JEYARAMAN M, MUTHU S, SHARMA S, et al. Nanofat: A therapeutic paradigm in regenerative medicine. World J Stem Cells. 2021;13(11):1733-1746.
[52] TONNARD P, VERPAELE A, CARVAS M. Fat Grafting for Facial Rejuvenation with Nanofat Grafts. Clin Plast Surg. 2020;47(1):53-62.
[53] XU P, YU Q, HUANG H, et al. Nanofat Increases Dermis Thickness and Neovascularization in Photoaged Nude Mouse Skin. Aesthetic Plast Surg. 2018;42(2):343-351.
[54] DING P, LU E, LI G, et al. Research progress on preparation, mechanism, and clinical application of nanofat. J Burn Care Res. 2022;43(5):1140-1144.
[55] WEINZIERL A, HARDER Y, SCHMAUSS D, et al. Boosting Tissue Vascularization: Nanofat as a Potential Source of Functional Microvessel Segments. Front Bioeng Biotechnol. 2022;10:820835.
[56] NG KLB, HSIEH MW, LIN YN, et al. Application of nanofat grafting to rescue a severe ischaemic hand with thromboangiitis obliterans: A case report about promising salvage procedure. Medicine (Baltimore). 2021;100(42):e27577.
[57] XU Y, DENG M, CAI Y, et al. Cell-Free Fat Extract Increases Dermal Thickness by Enhancing Angiogenesis and Extracellular Matrix Production in Nude Mice. Aesthet Surg J. 2020;40(8):904-913.
[58] RAGEH MA, EL-KHALAWANY M, IBRAHIM SMA. Autologous nanofat injection in treatment of scars: A clinico-histopathological study. J Cosmet Dermatol. 2021;20(10):3198-3204.
[59] LO FURNO D, TAMBURINO S, MANNINO G, et al. Nanofat 2.0: experimental evidence for a fat grafting rich in mesenchymal stem cells. Physiol Res. 2017;66(4):663-671.
[60] BI HS, ZHANG C, NIE FF, et al. Basic and Clinical Evidence of an Alternative Method to Produce Vivo Nanofat. Chin Med J (Engl). 2018;131(5):588-593.
[61] TRIVISONNO A, ALEXANDER RW, BALDARI S, et al. Intraoperative Strategies for Minimal Manipulation of Autologous Adipose Tissue for Cell- and Tissue-Based Therapies: Concise Review. Stem Cells Transl Med. 2019;8(12):1265-1271.
[62] SUN M, HE Y, ZHOU T, et al. Adipose Extracellular Matrix/Stromal Vascular Fraction Gel Secretes Angiogenic Factors and Enhances Skin Wound Healing in a Murine Model. Biomed Res Int. 2017;2017:3105780.
[63] YAO Y, DONG Z, LIAO Y, et al. Adipose Extracellular Matrix/Stromal Vascular Fraction Gel: A Novel Adipose Tissue-Derived Injectable for Stem Cell Therapy. Plast Reconstr Surg. 2017;139(4):867-879.
[64] ZHANG P, FENG J, LIAO Y, et al. Ischemic flap survival improvement by composition-selective fat grafting with novel adipose tissue derived product - stromal vascular fraction gel. Biochem Biophys Res Commun. 2018;495(3):2249-2256.
[65] ZHANG Y, CAI J, ZHOU T, et al. Improved Long-Term Volume Retention of Stromal Vascular Fraction Gel Grafting with Enhanced Angiogenesis and Adipogenesis. Plast Reconstr Surg. 2018;141(5):676e-686e.
[66] DENG C, HE Y, FENG J, et al. Extracellular matrix/stromal vascular fraction gel conditioned medium accelerates wound healing in a murine model. Wound Repair Regen. 2017;25(6):923-932.
[67] DENG C, WANG L, FENG J, et al. Treatment of human chronic wounds with autologous extracellular matrix/stromal vascular fraction gel: A STROBE-compliant study. Medicine (Baltimore). 2018;97(32):e11667.
[68] DENG C, HE Y, FENG J, et al. Conditioned medium from 3D culture system of stromal vascular fraction cells accelerates wound healing in diabetic rats. Regen Med. 2019;14(10):925-937.
[69] YANG Z, JIN S, HE Y, et al. Comparison of Microfat, Nanofat, and Extracellular Matrix/Stromal Vascular Fraction Gel for Skin Rejuvenation: Basic Research and Clinical Applications. Aesthet Surg J. 2021;41(11):NP1557-NP1570. |