| [1] 孙安科,陈文弦,崔鹏程,等.同种异体工程化软骨的构建和修复甲状软骨缺损的实验研究[J].中华耳鼻咽喉科杂志, 2001,36(4):278-280.[2] 孙安科,陈文弦,崔鹏程,等.同种异体软骨细胞-聚羟基乙酸复合物修复喉软骨缺损[J].现代康复, 2001,5(7): 43-44.[3] 孙安科,孙靖,孙伟,等.无纺网与多孔海绵状材料作为软骨组织工程支架的适用性及体内降解性[J].中国组织工程研究,2014,18(8):1172-1178.[4] 孙安科,裴国献,周国平,等.改良以聚羟基乙酸为支架同种异体组织工程化塑形软骨的构建[J].第一军医大学学报, 2002,22(11):996-999.[5] Bhavana K,Tyragi I,Ramani MK.Laryngotracheal reconstruction using iliac crest graft:an institutional experience.Indian J Otolaryngol Head Neck. 2010; 62(1):75-78.[6] 杨大鉴,黄定强,胥方元,等.兔骨髓间充质干细胞及聚羟基乙酸支架材料构建人工软骨的可行性[J].中国组织工程研究与临床康复,2007,11(14):2761-2764.[7] 孙安科,裴国献,陈文弦,等.聚羟基乙酸负载软骨细胞修复同种异体甲状软骨缺损[J].中华耳鼻咽喉科杂志, 2003, 38(5):347-350.[8] 李军政,成诗银,崔鹏程,等.低温冻存同种异体软骨细胞在喉功能重建中的应用[J].中国临床康复, 2005,9(2): 45-47.[9] 李军政.低温冻存软骨细胞构建组织工程化软骨及组织工程化软骨的低温冻存[D].第四军医大学,2005.[10] 吴海涛,钟翠平,王薇,等.软骨细胞三维支架短期固定培养实验研究[J].耳鼻咽喉头颈外科,2000,7(5):298-301.[11] 杨大鉴,黄定强,胥方元,等.骨髓间充质干细胞-支架复合体向软骨诱导分化的实验研究[J].泸州医学院学报, 2005,28(5):394-396.[12] 倪云峰,李小飞,刘源,等.兔骨髓基质干细胞与软骨细胞混和培养体内成软骨[J].中国组织工程研究与临床康复, 2008,12(16):3185-3188.[13] 崔玉明,伍骥,胡蕴玉,等.聚乳酸/聚羟基乙酸复合骨形成蛋白修复兔关节软骨缺损[J].中国修复重建外科杂志, 2007,21(11):1233-1237.[14] Kim HKW,Moran ME,Salter RB.The potential for regeneration of articular cartilage in defects created by chondral shaving and subchondral abrasion.J Bone Joint Surg Am. 1991;73(9):1301-1315.[15] 吴玉家,江华,周广东,等.构建带内支撑组织工程软骨的实验研究[J].中华整形外科杂志,2007,23(4):328-331.[16] 孙安科,陈文弦,李东军,等.聚羟基乙酸无纺网设计在软骨组织工程中的适用研究[J].现代康复,2001,5(6): 38-39.[17] 李德保,田甜,章庆国等.膨体聚四氟乙烯(ePTFE)内支撑组织工程软骨的构建实验研究[J].中国美容医学, 2009, 18(6):823-826.[18] 韩志军,任华.两种聚羟基乙酸支架与猪软骨样细胞体外相容性比较[J].协和医学杂志,2011,2(1):42-45.[19] 王永春,沈尊理,钱鋆,等.冻干骨和PLGA材料表面软骨细胞增殖的形态学观察比较[J].组织工程与重建外科杂志, 2007,3(1):19-21,51.[20] 崔玉明,伍骥,胡蕴玉,等.骨髓基质细胞源性软骨细胞复合聚乳酸/聚羟基乙酸共聚物修复兔关节软骨缺损[J].中国组织工程研究与临床康复, 2009,13(51):10049- 10054.[21] 李红喜,张睿,李华哲,等.软骨细胞联合BMP/bFGF移植对关节软骨损伤的修复作用[J].现代生物医学进展, 2013, 13(22):4237-4241.[22] Kiss A,Cucchiarini M,Menger MD,et al.Enamel matrix derivative inhibits proteoglycan production and articular cartilage repair, delays the restoration of the subchondral bone and induces changes of the synovial membrane in a lapine osteochondral defect model in vivo.J Tissue Eng Regen M.2014;8(1):41-49.[23] Lohmann CH,Schwartz Z,Niederauer GG,et al. Pretreatment with platelet derived growth factor-BB modulates the ability of costochondral resting zone chondrocytes incorporated into PLA/PGA scaffolds to form new cartilage in vivo.Biomaterials. 2000;21(1):49-61.[24] Lim SY,Mun GH,Hyon WS,et al.The elevation of the constructed auricle with a temporoparietal fascial flap wrapping a resorbable plate.J Plast Reconstr Aesthet surg.2006;59(5):505-509.[25] Homicz MR,Chia SH,Schumacher BL,et al.Human septal chondrocyte redifferentiation in alginate, polyglycolic acid scaffold, and monolayer culture. Laryngoscope.2003;113(1):25-32.[26] 郑信民,董淑芬,胡永声,等.人同种软骨移植的临床及实验室观察[J].中华整形烧伤外科杂志,1990,37(2):91-93.[27] Donald PJ.Cartilage grafting in facial reconstruction with special consideration of irradiated grafts. Laryngoscope.1986;96(7):786-807. [28] 夏万尧,刘伟,刘天一,等.应用骨髓基质干细胞体外构建组织工程化管状软骨的实验研究[J].中华显微外科杂志, 2005,28(4):328-330,插图4-4.[29] 苗春雷,周广东,刘天一,等.软骨细胞与骨髓基质细胞共培养体外构建软骨的初步研究[J].上海第二医科大学学报, 2004,24(4):246-249,283.[30] 孙晋客,刘锋,范卫民,等.不同材料包埋的PGA支架对软骨细胞体外培养的影响[J].江苏医药, 2006,32(7): 642-644, 插4.[31] 欧阳彬,范卫民,马益民,等.壳聚糖、Ⅱ型胶原和PGA三种支架体外构建组织工程软骨的比较研究[J].江苏医药, 2007,33(9):904-906[32] 倪云峰,李小飞,刘源,等.兔骨髓基质干细胞与软骨细胞共培养体内成软骨的实验观察[J].第四军医大学学报, 2006,27(7):612-614.[33] Jiang J,Zhao Z,Guoyu L,et al.Syntheses and evaluation of copolymer 6-aminohexanoic acid and 4R-hydroxy-L-proline for bone repair//Materials Engineering and Automatic Control.2012:491-496.[34] Poologasundarampillai G,Ionescu C,Tsigkou O,et al.Synthesis of bioactive class II poly(γ-glutamic acid)/silica hybrids for bone regeneration.J Mater Chem.2010;20(40):8952-8961.[35] Thomson RC,Yaszemski MJ,Powers JM et al. Hydroxyapatite fiber reinforced poly(alpha-hydroxy ester) foams for bone regeneration.Biomaterials. 1998;19(21):1935-1943.[36] I.Raizer,W.Chrzanowski,W.Binias et al.Nano Hydroxyapatie Polylactic Acid Electrospun Scaffolds for Bone Tissue Engineering[C].//23rd European conference on biomaterials 2010.2010:449-449.[37] Hollinger JO,Mayer M,Buck D.Poly(α-hydroxy acid) carrier for deliverking recombinant human bone morphogenetic protein-2 for bone regeneration.J Controll Release.1996;39(39):287.[38] Fukuda A,Kato K,Hasegawa M,et al.Enhanced repair of large osteochondral defects using a combination of artificial cartilage and basic fibroblast growth factor. Biomaterials.2005;26(20):4301-4308.[39] Tang C,Xu Y,Jin C,et al.Feasibility of Autologous Bone Marrow Mesenchymal Stem Cell-Derived Extracellular Matrix Scaffold for Cartilage Tissue Engineering. Artificial Organs.2013;37(12):E179-E190.[40] 崔玉明,伍骥,胡蕴玉,等.聚乳酸/聚羟基乙酸共聚物修复髌股关节软骨缺损[J].中国组织工程研究与临床康复, 2011,15(16):2877-2880. [41] Lee CC,Lo Y,Ho LJ,et al.A New Application of Parallel Synthesis Strategy for Discovery of Amide-Linked Small Molecules as Potent Chondroprotective Agents in TNF-α-Stimulated Chondrocytes.PLoS One. 2016; 11(3):e0149317.[42] Anbarasan S,Baraneedharan U,Paul SF,et al.Low dose short duration pulsed electromagnetic field effects on cultured human chondrocytes: An experimental study.Indian J Orthop.2016;50(1):87-93. [43] Mueller M,Weinmann D,Toegel S,et al.Compounds from Caesalpinia sappan with anti-inflammatory properties in macrophages and chondrocytes.Food Funct. 2016;7(3):1671-1679.[44] Dai X,Li Y,Zhang R,et al.Effects of sodium selenite on c-Jun N-terminal kinase signalling pathway induced by oxidative stress in human chondrocytes and c-Jun N-terminal kinase expression in patients with Kashin-Beck disease, an endemic osteoarthritis.Br J Nutr.2016:1-9. [Epub ahead of print][45] Huang Z,Du S,Huang L,et al.Leptin promotes apoptosis and inhibits autophagy of chondrocytes through upregulating Lysyl oxidase-like 3 during osteoarthritis pathogenesis.Osteoarthritis Cartilage. 2016.pii: S1063-4584(16)01042-6. [46] Recha-Sancho L,Semino CE.Heparin based self-assembling peptide scaffold reestablish chondrogenic phenotype of expanded de-differentiated human chondrocytes.J Biomed Mater Res A.2016.doi: 10.1002/jbm.a.35699. [Epub ahead of print][47] Huang Z,Li J,Du S,et al.Effects of UCP4 on the Proliferation and Apoptosis of Chondrocytes: Its Possible Involvement and Regulation in Osteoarthritis. PLoS One.2016;11(3):e0150684.[48] 48 Yoon HI,Yhee JY,Na JH,et al.Bioorthogonal Copper Free Click Chemistry for Labeling and Tracking of Chondrocytes In Vivo.Bioconjug Chem. 2016. [Epub ahead of print][49] Cizelj I,Dušani? D,Ben?ina D,et al.Mycoplasma and host interaction: In vitro gene expression modulation in Mycoplasma synoviae and infected chicken chondrocytes. Acta Vet Hung.2016;64(1):26-37. [50] Yeh HY,Hsieh FY,Hsu SH.Self-patterning of adipose-derived mesenchymal stem cells and chondrocytes cocultured on hyaluronan-grafted chitosan surface.Biointerphases. 2016 5;11(1):011011.[51] Xu HG,Ma MM,Zheng Q,et al.P120-Catenin Protects Endplate Chondrocytes from Intermittent Cyclic Mechanical Tension Induced Degeneration by Inhibiting the Expression of RhoA/ROCK-1 Signaling Pathway.Spine (Phila Pa 1976).2016.[Epub ahead of print] |
.jpg)

.jpg)
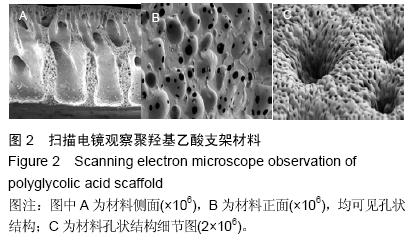
.jpg)