[1] CLARKE B. Normal bone anatomy and physiology. Clin J Am Soc Nephrol. 2008;3 Suppl 3(Suppl 3):S131-S139.
[2] XUE N, DING X, HUANG R, et al. Bone tissue engineering in the treatment of bone defects. Pharmaceuticals (Basel). 2022. doi: 10.3390/ph15070879.
[3] PERIĆ K, RIDER P, ALKILDANI S, et al. An introduction to bone tissue engineering. Int J Artif Organs. 2020;43(2):69-86.
[4] YONG KW, CHOI JR, CHOI JY, et al. Recent advances in mechanically loaded human mesenchymal stem cells for bone tissue engineering. Int J Mol Sci. 2020;21(16):5816.
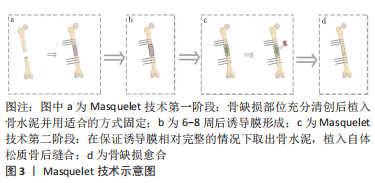
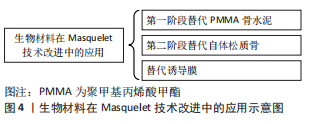
[5] MATHIEU L, MOURTIALON R, DURAND M, et al. Masquelet technique in military practice: specificities and future directions for combat-related bone defect reconstruction. Mil Med Res. 2022;9(1):48.
[6] DALISSON B, CHARBONNIER B, AOUDE A, et al. Skeletal regeneration for segmental bone loss: vascularised grafts, analogues and surrogates. Acta Biomater. 2021;136:37-55.
[7] LIODAKIS E, GIANNOUDIS VP, SEHMISCH S, et al. Bone defect treatment: does the type and properties of the spacer affect the induction of Masquelet membrane? Evidence today. Eur J Trauma Emerg Surg. 2022; 48(6):4403-4424.
[8] MASQUELET AC. Induced membrane technique: pearls and pitfalls. J Orthop Trauma. 2017;31 Suppl 5:S36-S38.
[9] KLEIN C, MONET M, BARBIER V, et al. The Masquelet technique: current concepts, animal models, and perspectives. J Tissue Eng Regen Med. 2020; 14(9):1349-1359.
[10] 吴斗,刘强.Masquelet技术修复骨缺损的实验研究现状和展望[J].中华实验外科杂志,2020,37(11):1983-1987.
[11] MASQUELET AC, FITOUSSI F, BEGUE T, et al. Reconstruction of the long bones by the induced membrane and spongy autograft. Ann Chir Plast Esthet. 2000;45(3):346-353.
[12] MASQUELET AC, BEGUE T. The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am. 2010;41(1): 27-37.
[13] WANG W, ZUO R, LONG H, et al. Advances in the Masquelet technique: myeloid-derived suppressor cells promote angiogenesis in PMMA-induced membranes. Acta Biomater. 2020;108:223-236.
[14] MCCONOUGHEY SJ, HOWLIN RP, WISEMAN J, et al. Comparing PMMA and calcium sulfate as carriers for the local delivery of antibiotics to infected surgical sites. J Biomed Mater Res B Appl Biomater. 2015;103(4):870-877.
[15] MASQUELET A, KANAKARIS N K, OBERT L, et al. Bone repair using the masquelet technique. J Bone Joint Surg Am. 2019;101(11):1024-1036.
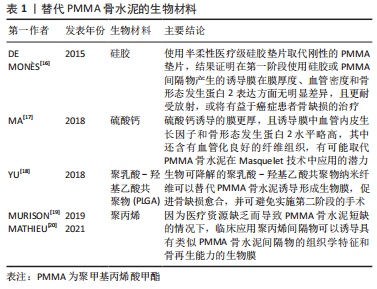
[16] de MONÈS E, SCHLAUBITZ S, OLIVEIRA H, et al. Comparative study of membranes induced by PMMA or silicone in rats, and influence of external radiotherapy. Acta Biomater. 2015;19:119-127.
[17] MA YF, JIANG N, ZHANG X, et al. Calcium sulfate induced versus PMMA-induced membrane in a critical-sized femoral defect in a rat model. Sci Rep. 2018;8(1):637.
[18] YU Y, WU R, LEE D, et al. Artificial membrane induced by novel biodegradable nanofibers in the masquelet procedure for treatment of segmental bone defects. J Nanomater. 2018;2018:8246571.
[19] MURISON J C, PFISTER G, AMAR S, et al. Metacarpal bone reconstruction by a cementless induced membrane technique. Hand Surg Rehabil. 2019; 38(2):83-86.
[20] MATHIEU L, MURISON JC, de ROUSIERS A, et al. The masquelet technique: can disposable polypropylene syringes be an alternative to standard PMMA spacers? A rat bone defect model. Clin Orthop Relat Res. 2021; 479(12):2737-2751.
[21] MCBRIDE-GAGYI S, TOTH Z, KIM D, et al. Altering spacer material affects bone regeneration in the Masquelet technique in a rat femoral defect. J Orthop Res. 2018. doi: 10.1002/jor.23866.
[22] TOTH Z, ROI M, EVANS E, et al. Masquelet technique: effects of spacer material and micro-topography on factor expression and bone regeneration. Ann Biomed Eng. 2019;47(1):174-189.
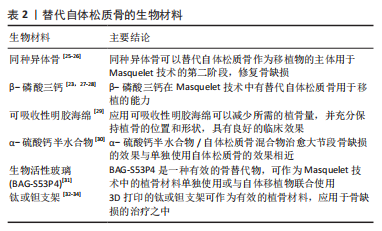
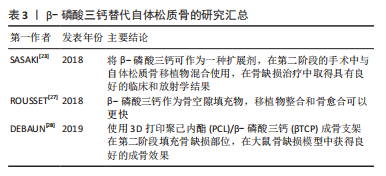
[23] SASAKI G, WATANABE Y, MIYAMOTO W, et al. Induced membrane technique using beta-tricalcium phosphate for reconstruction of femoral and tibial segmental bone loss due to infection: technical tips and preliminary clinical results. Int Orthop. 2018;42(1):17-24.
[24] LE BARON M, VIVONA JP, MAMAN P, et al. Can the reamer/irrigator/aspirator system replace anterior iliac crest grafting when treating long bone nonunion? Orthop Traumatol Surg Res. 2019;105(3):529-533.
[25] NICCOLAI F, Di MENTO L, MOCCHI M, et al. Modified masquelet’s technique with nail and allograft: a case report. Injury. 2018;49 Suppl 4:S21-S24.
[26] VIALE GJ, GARABANO G, PESCIALLO C, et al. Structural allograft and induced membrane technique for treatment of 10-cm segmental femoral bone defect: a case report. JBJS Case Connect. 2021. doi: 10.2106/JBJS.CC.21.00372.
[27] ROUSSET M, WALLE M, CAMBOU L, et al. Chronic infection and infected non-union of the long bones in paediatric patients: preliminary results of bone versus beta-tricalcium phosphate grafting after induced membrane formation. Int Orthop. 2018;42(2):385-393.
[28] DEBAUN MR, STAHL AM, DAOUD AI, et al. Preclinical induced membrane model to evaluate synthetic implants for healing critical bone defects without autograft. J Orthop Res. 2019;37(1):60-68.
[29] CHO JW, KIM J, CHO WT, et al. Circumferential bone grafting around an absorbable gelatin sponge core reduced the amount of grafted bone in the induced membrane technique for critical-size defects of long bones. Injury. 2017;48(10):2292-2305.
[30] MENG ZL, WU ZQ, SHEN BX, et al. Reconstruction of large segmental bone defects in rabbit using the Masquelet technique with α-calcium sulfate hemihydrate. J Orthop Surg Res. 2019;14(1):192.
[31] AURÉGAN JC, VILLAIN B, GLOMBITZA M, et al. Utilisation of bioactive glass S53P4 inside an induced membrane for severe bone defect with high risk of infection: a multi-center preliminary experience. Injury. 2022;53 Suppl 2: S13-S19.
[32] QIAO S, WU D, LI Z, et al. The combination of multi-functional ingredients-loaded hydrogels and three-dimensional printed porous titanium alloys for infective bone defect treatment. J Tissue Eng. 2020;11:1542272091.
[33] GAVASKAR AS, PARTHASARATHY S, BALAMURUGAN J, et al. A load-sharing nail-cage construct may improve outcome after induced membrane technique for segmental tibial defects. Injury. 2020;51(2):510-515.
[34] WU Y, SHI X, ZI S, et al. The clinical application of customized 3D-printed porous tantalum scaffolds combined with Masquelet’s induced membrane technique to reconstruct infective segmental femoral defect. J Orthop Surg Res. 2022;17(1):479.
[35] JIANG SD, JIANG LS, DAI LY. Surgical treatment of calcaneal fractures with use of beta-tricalcium phosphate ceramic grafting. Foot Ankle Int. 2008; 29(10):1015-1019.
[36] DAI LY, JIANG LS. Single-level instrumented posterolateral fusion of lumbar spine with beta-tricalcium phosphate versus autograft: a prospective, randomized study with 3-year follow-up. Spine (Phila Pa 1976). 2008;33(12): 1299-1304.
[37] GUPTA S, MALHOTRA A, JINDAL R, et al. Role of beta tri-calcium phosphate-based composite ceramic as bone-graft expander in Masquelet’s-induced membrane technique. Indian J Orthop. 2019;53(1):63-69.
[38] TANNER MC, HELLER R, WESTHAUSER F, et al. Evaluation of the clinical effectiveness of bioactive glass (S53P4) in the treatment of non-unions of the tibia and femur: study protocol of a randomized controlled non-inferiority trial. Trials. 2018;19(1):299.
[39] ALFORD AI, NICOLAOU D, HAKE M, et al. Masquelet’s induced membrane technique: Review of current concepts and future directions. J Orthop Res. 2021;39(4):707-718.
[40] KARIMI GE, MEIMANDI-PARIZI A, ORYAN A, et al. Effects of combination of BMP7, PFG, and autograft on healing of the experimental critical radial bone defect by induced membrane (Masquelet) technique in rabbit. Arch Bone Jt Surg. 2021;9(5):585-597.
[41] ARıCAN G, ÖZMERIÇ A, FıRAT A, et al. Micro-ct findings of concentrated growth factors (cgf) on bone healing in masquelet’s technique-an experimental study in rabbits. Arch Orthop Trauma Surg. 2022;142(1):83-90.
[42] 高峻青,王朝辉,詹晓欢,等.Masquelet技术联合富血小板血浆修复胫骨大段骨缺损[J].中华创伤骨科杂志,2020,22(4):315-316.
[43] LEIBLEIN M, WINKENBACH A, KOCH E, et al. Impact of scaffold granule size use in Masquelet technique on periosteal reaction: a study in rat femur critical size bone defect model. Eur J Trauma Emerg Surg. 2022;48(1): 679-687.
[44] VIATEAU V, BENSIDHOUM M, GUILLEMIN G, et al. Use of the induced membrane technique for bone tissue engineering purposes: animal studies. Orthop Clin North Am. 2010;41(1):49-56.
[45] HENRICH D, SEEBACH C, NAU C, et al. Establishment and characterization of the Masquelet induced membrane technique in a rat femur critical-sized defect model. J Tissue Eng Regen Med. 2016;10(10):E382-E396.
[46] AHO OM, LEHENKARI P, RISTINIEMI J, et al. The mechanism of action of induced membranes in bone repair. J Bone Joint Surg Am. 2013;95(7):597-604.
[47] REN L, KANG Y, BROWNE C, et al. Fabrication, vascularization and osteogenic properties of a novel synthetic biomimetic induced membrane for the treatment of large bone defects. Bone. 2014;64:173-182.
[48] RICCI E, VANOSI G, LINDENMAIR A, et al. Anti-fibrotic effects of fresh and cryopreserved human amniotic membrane in a rat liver fibrosis model. Cell Tissue Bank. 2013;14(3):475-488.
[49] GINDRAUX F, RONDOT T, de BILLY B, et al. Similarities between induced membrane and amniotic membrane: novelty for bone repair. Placenta. 2017;59:116-123.
[50] FENELON M, ETCHEBARNE M, SIADOUS R, et al. Comparison of amniotic membrane versus the induced membrane for bone regeneration in long bone segmental defects using calcium phosphate cement loaded with BMP-2. Mater Sci Eng C Mater Biol Appl. 2021;124:112032.
[51] VITACOLONNA M, MULARCZYK M, HERRLE F, et al. Effect on the tensile strength of human acellular dermis (Epiflex®) of in-vitro incubation simulating an open abdomen setting. BMC Surg. 2014;14:7.
[52] VERBOKET RD, LEIBLEIN M, JANKO M, et al. From two stages to one: acceleration of the induced membrane (Masquelet) technique using human acellular dermis for the treatment of non-infectious large bone defects. Eur J Trauma Emerg Surg. 2020;46(2):317-327.
[53] DIMITRIOU R, MATALIOTAKIS GI, CALORI GM, et al. The role of barrier membranes for guided bone regeneration and restoration of large bone defects: current experimental and clinical evidence. BMC Med. 2012;10:81.
[54] TARCHALA M, ENGEL V, BARRALET J, et al. A pilot study: alternative biomaterials in critical sized bone defect treatment. Injury. 2018;49(3):523-531.
[55] OH Y, YOSHII T, OKAWA A. Ankle arthrodesis using a modified Masquelet induced membrane technique for open ankle fracture with a substantial osteochondral defect: a case report of novel surgical technique. Injury. 2019;50(11):2128-2135.
[56] NAU C, SEEBACH C, TRUMM A, et al. Alteration of Masquelet’s induced membrane characteristics by different kinds of antibiotic enriched bone cement in a critical size defect model in the rat’s femur. Injury. 2016;47(2): 325-334.
[57] WANG X, LUO F, HUANG K, et al. Induced membrane technique for the treatment of bone defects due to post-traumatic osteomyelitis. Bone Joint Res. 2016;5(3):101-105.
[58] HAN W, SHEN J, WU H, et al. Induced membrane technique: advances in the management of bone defects. Int J Surg. 2017;42:110-116. |