|
[1] NUNLEY PD, CORIC D, FRANK KA, et al. Cervical disc arthroplasty: current evidence and real-world application. Neurosurgery. 2018;83(6):1087-1106.
[2] YANG Y, SHI B, DUAN Y, et al. Anatomic morphology and clinical significance of intraforaminal ligaments of the cervical spine. Clin Anat. 2019;32(5):654-660.
[3] 袁野,郭晓丹,姜里强,等.颈胸段脊柱手术前方入路的应用解剖[J].解剖学杂志,2017,40(4):453-455.
[4] RYU JI, HAN MH, KIM JM, et al. Cervical epidural hematoma that induced sudden paraparesis after cervical spine massage: case report and literature review. World Neurosurg. 2018;112:217-220.
[5] RADCLIFF K, ONG KL, LOVALD S, et al. Cervical Spine Surgery Complications and Risks in the Elderly. Spine (Phila Pa 1976). 2017;42(6):E347-E354.
[6] SMITH JS, FU KM, POLLY DJ, et al. Complication rates of three common spine procedures and rates of thromboembolism following spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976). 2010;35(24):2140-2149.
[7] CARLSON BC, ROBINSON WA, WANDERMAN NR, et al. A Review and Clinical Perspective of the Impact of Osteoporosis on the Spine. Geriatr Orthop Surg Rehabil.2019;10:1467854505.
[8] WILLNER D, SPENNATI V, STOHL S, et al. Spine surgery and blood loss: systematic review of clinical evidence. Anesth Analg. 2016;123(5):1307-1315.
[9] LAPAGE KG, WOUTERS PF. The patient with hypertension undergoing surgery. Curr Opin Anaesthesiol. 2016;29(3):397-402.
[10] DELESKOG L, LAURSEN NO, NIELSEN BR, et al. Vertebral fracture assessment by DXA is inferior to X-ray in clinical severe osteoporosis. Osteoporos Int. 2016;27(7):2317-2326.
[11] HAREL R, STYLIANOU P, KNOLLER N. Cervical spine surgery: approach-related complications. World Neurosurg. 2016;94:1-5.
[12] SMORGICK Y, BAKER KC, BACHISON CC, et al. Hidden blood loss during posterior spine fusion surgery. Spine J. 2013;13(8): 877-881.
[13] WU YS, ZHANG H, ZHENG WH, et al. Hidden blood loss and the influential factors after percutaneous kyphoplasty surgery. Eur Spine J. 2017;26(7):1878-1883.
[14] UHRENHOLT L, CHARLES AV, GREGERSEN M, et al. Histological osteoarthritic changes in the human cervical spine facet joints related to age and sex. Spine (Phila Pa 1976). 2018; 43(12):E689-E696.
[15] ZHENG B, HAO D, GUO H, et al. ACDF vs TDR for patients with cervical spondylosis - an 8 year follow up study. BMC Surg. 2017; 17(1):113.
[16] MUZEVIC D, SPLAVSKI B, BOOP FA, et al. Anterior cervical discectomy with instrumented allograft fusion: lordosis restoration and comparison of functional outcomes among patients of different age groups. World Neurosurg. 2018;109:e233-e243.
[17] LIM S, CARABINI LM, KIM RB, et al. Evaluation of American Society of Anesthesiologists classification as 30-day morbidity predictor after single-level elective anterior cervical discectomy and fusion. Spine J. 2017;17(3):313-320.
[18] GOODNOUGH LT, RUDNICK S, PRICE TH, et al. Increased preoperative collection of autologous blood with recombinant human erythropoietin therapy. N Engl J Med.1989;321(17): 1163-1168.
[19] PAUYO T, VERMA N, MARWAN Y, et al. Canadian Consensus for the Prevention of Blood Loss in Spine Surgery. Spine (Phila Pa 1976).2017;42(1):E50-E55.
[20] PATEL N, BAGAN B, VADERA S, et al. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine. 2007; 6(4):291-297.
[21] NARAIN AS, HIJJI FY, HAWS BE, et al. Impact of body mass index on surgical outcomes, narcotics consumption, and hospital costs following anterior cervical discectomy and fusion. J Neurosurg Spine. 2018;28(2):160-166.
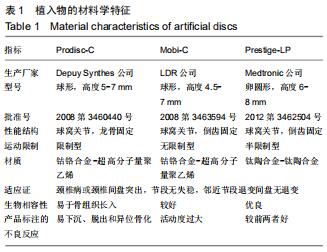
[22] TUREL MK, KEROLUS MG, ADOGWA O, et al. Cervical arthroplasty: what does the labeling say? Neurosurg Focus. 2017;42(2):E2.
[23] BUCKLAND AJ, BAKER JF, ROACH RP, et al. Cervical disc replacement - emerging equivalency to anterior cervical discectomy and fusion. Int Orthop. 2016;40(6):1329-1334.
[24] LANDI A, GREGORI F, MAROTTA N, et al. Efficacy, security, and manageability of gelified hemostatic matrix in bleeding control during thoracic and lumbar spine surgery: floseal versus surgiflo. J Neurol Surg A Cent Eur Neurosurg. 2016;77(2):139-143.
[25] BURGER W, CHEMNITIUS JM, KNEISSL GD, et al. Low-dose aspirin for secondary cardiovascular prevention - cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation - review and meta-analysis. J Intern Med. 2005; 257(5):399-414.
[26] EPSTEIN NE. When to stop anticoagulation, anti-platelet aggregates, and non-steroidal anti-inflammatories (NSAIDs) prior to spine surgery. Surg Neurol Int. 2019;10:45.
[27] THAKUR S, RIYAZ B, PATIL A, et al. Novel drug delivery systems for NSAIDs in management of rheumatoid arthritis: An overview. Biomed Pharmacother. 2018;106:1011-1023.
[28] CHOI SH, CHO JH, HWANG CJ, et al. Preoperative Radiographic parameters to predict a higher pseudarthrosis rate after anterior cervical discectomy and fusion. Spine (Phila Pa 1976).2017; 42(23):1772-1778.
[29] PENZKOFER R, HOFBERGER S, SPIEGL U, et al. Biomechanical comparison of the end plate design of three vertebral body replacement systems. Arch Orthop Trauma Surg,2011;131(9):1253-1259.
[30] RONG X, LOU J, LI H, et al. How to choose when implants of adjacent height both fit the disc space properly in single-level cervical artificial disc replacement. Medicine (Baltimore).2017; 96(29):e6954.
[31] WANG H, SUN W, FU D, et al. Update on biomaterials for prevention of epidural adhesion after lumbar laminectomy. J Orthop Translat. 2018;13:41-49.
[32] 金永明,郑嘉寅,张骏,等.脊柱转移性肿瘤后路360度减压内固定手术时间和出血量的影响因素分析[J].浙江医学,2014,36(6):489-493.
[33] 钱邦平,邱勇,乔军,等.全椎弓根螺钉矫正青少年特发性脊柱侧凸术中出血量及手术时间的影响因素分析[J].解剖与临床,2011,16(2): 124-126.
[34] 刘丰,尹庆水,吴锐辉,等.颈椎前路减压与椎内静脉丛相关的应用解剖学研究[J].中国临床解剖学杂志,2008,26(3):262-264.
|