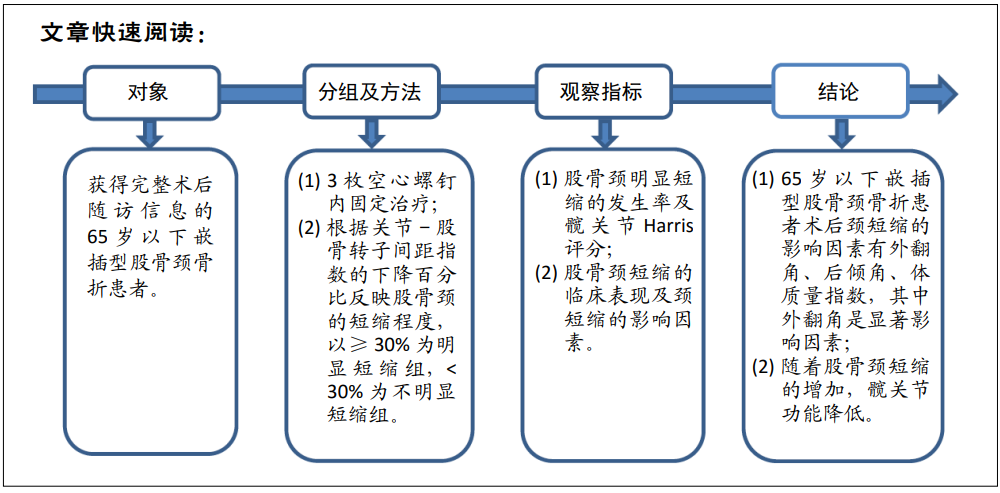
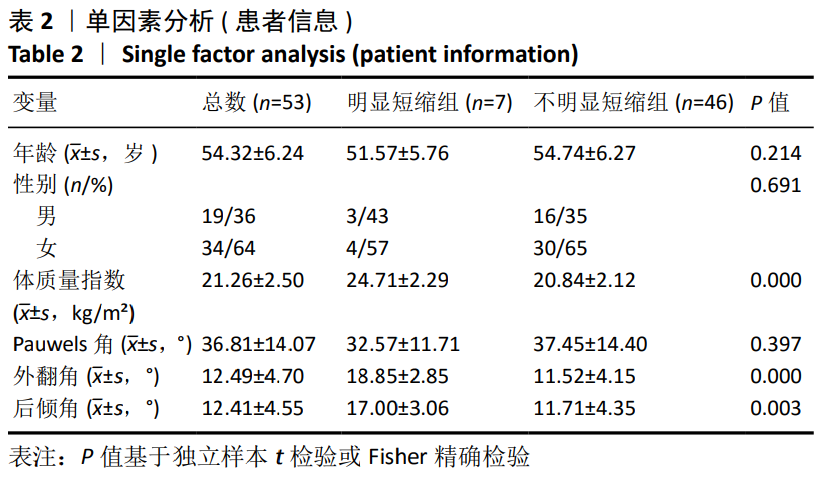
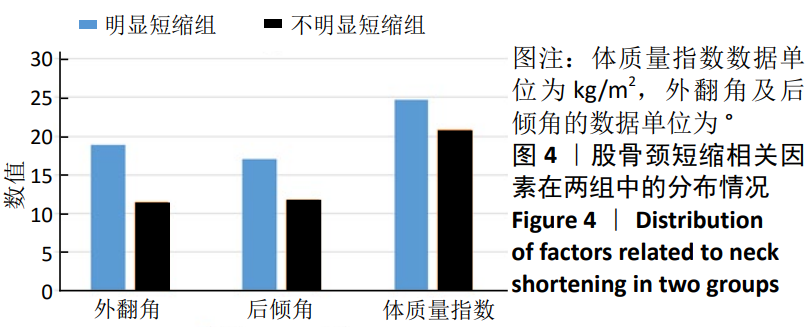
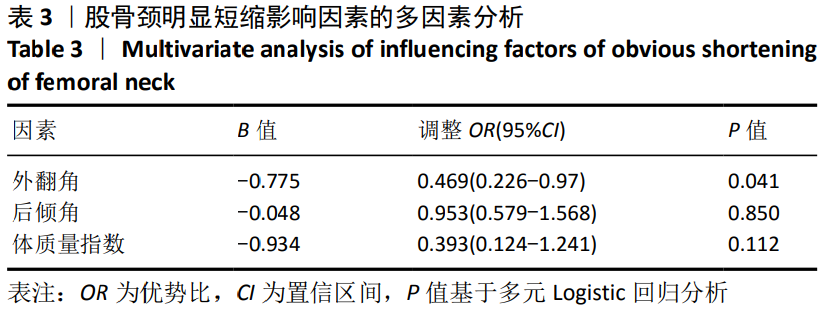
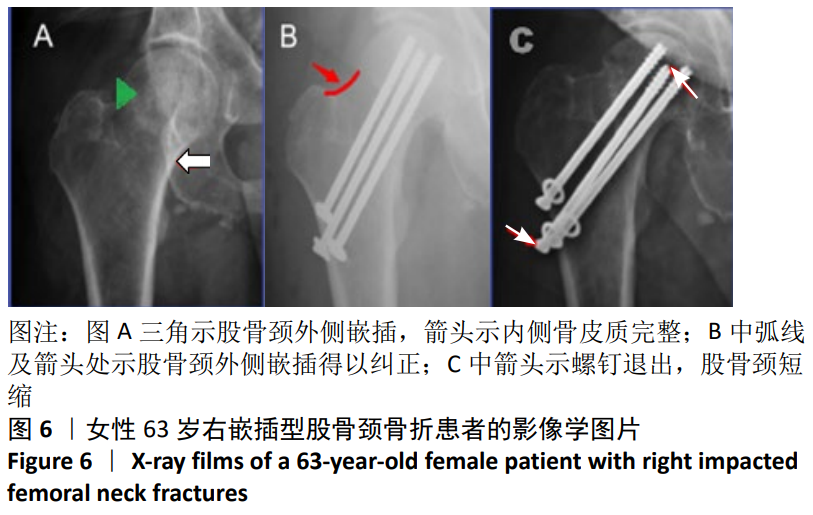
嵌插型股骨颈骨折的治疗方式有手术治疗和保守治疗。若股骨头有旋转或嵌插部分骨质量差,可能会发生继发性移位[7];在已发表的研究中,二次位移的概率为33%-44.3%[7-9],多个平行螺钉内固定术已被认为是治疗无移位或轻度移位股骨颈骨折的首选方法,因为它提供了额外的稳定性,并允许早期负重;内固定也消除了在保守治疗过程中8%-15%的患者可能发生的再移位风险[10]。在此次研究中证明了内固定治疗65岁以下嵌插型股骨颈骨折患者的良好结果,其中53例患者全部骨愈合,无股骨头坏死等不良事件发生;但在随访过程中,发现了部分患者股骨颈明显短缩(发生率13.2%);单因素分析发现外翻角、后倾角和体质量指数在两组中差异有显著性意义,Logistic回归分析发现外翻角是明显短缩的独立预测因子。
3.1 颈短缩的发生率 作者回顾了相关文献,无论老年人还是年轻人,股骨颈骨折术后愈合过程中的颈短缩是常见的。ZLOWODSKI等[11]在多个松质骨螺钉固定未移位的股骨颈骨折中发现,34%为无/轻度缩短(<5 mm),36%为中度缩短(5-10 mm),30%为重度缩短(>10 mm);STOCKTON 等[12]在应用多个松质螺钉或滑动髋螺钉治疗≤60岁的年轻患者时发现中度短缩(5-10 mm)率为22%,重度短缩率(>10 mm)为32%;这两项研究在重度短缩率上无明显差异。SLOBOGEAN等[10]发现55岁以下的股骨颈骨折患者接受多个松质螺钉固定后,有22.8%的患者中度缩短,12.9%的患者有严重缩短。在最近的一项多中心对照试验中,患者年龄大于55岁,有1/3的患者短缩超过5 mm[13]。由于测量方法及描述股骨颈短缩程度的方式不一致,此次研究结果不能与上述文献做比较。SUNG等[14]在对83例嵌插型股骨颈骨折患者的回顾性研究中发现,有13例(15.7%)患者明显短缩,与此次研究结果(13.2%)相似。
股骨颈骨折最常见的内固定技术是应用滑动髋螺钉和多个套管平行螺钉,骨折断端沿这种内植物滑动加压,进而促进骨折愈合,所以造成的股骨颈短缩是被允许的,也是常见的。虽然滑动在生物力学上对骨折愈合是有益的,但还没有证明在负重过程中的动态骨折压缩,以及在骨折固定过程中实现的压缩是骨愈合所必需的[15]。
在此次研究中,测量股骨颈的短缩程度是在末次随访中进行的,所有病例的颈短缩测量时间均大于12个月,这在以往的研究中证明是可行的。RAGNARSSON等[16]发现骨折在6个月内恢复稳定,但那些持续微运动和缩短9-12个月的骨折容易发生骨坏死。BORAIAH等[17]认为至少6个月的X射线片随访是可行的,因为骨折愈合前的任何短缩都将在这个时间点截止。THOMAS等[18]在一项长期随访中发现,术后5年(中位数66.5个月)与术后3个月测量的颈缩短无明显差异。
3.2 颈短缩的影响因素 目前的研究表明股骨颈短缩的影响因素有年龄、性别、骨密度、体质量指数、手术方式、骨折移位程度及骨折线的方向(Pauwels角)等,但是在各个研究中存在分歧。在此次研究中,为了降低干扰因素对结果的影响,作者统一了手术方式、骨折类型与年龄限定(<65岁),结果发现外翻角、后倾角、体质量指数与嵌插型股骨颈骨折的颈缩短有关,Logistic回归分析发现外翻角是显著影响因子(P < 0.05)。
在先前的研究中认为,Pauwels分类是股骨颈短缩的影响因素[10,19-21],与Pauwels 1型和2型相比,Pauwels 3型骨折具有较高的运动倾向,Pauwels分级较高的骨折导致股骨缩短程度明显增大(3 mm vs. 4 mm vs. 7 mm,P < 0.05)[20];而在此次研究中,颈短缩与Pauwels分型无关。分析原因如下:①Pauwels分类最初被确定为股骨颈骨折稳定性的因素,根据最近的文献,这一因素似乎不比Garden分类更重要[19]。早在1998年PARKER等[22]就提出Pauwels角的测量在股骨颈骨折治疗中没有价值,对于非手术治疗的未移位骨折,角度越大,可能表明骨折更有可能移位;但对于正在手术治疗的骨折,它没有任何证明价值。但是在后续的研究中,如上所述,仍然观察到Pauwels分型对股骨颈骨折预后的影响,虽然对PARKER的结论不能持肯定态度,但至少发现Pauwels分型对临床的局限性。根据结果而言,Pauwels分类对65岁以下嵌插型股骨颈骨折术后的颈缩短没有影响。②Pauwels 3型股骨颈骨折在嵌插型股骨颈骨折中分布较少,仅占12.79%-17.7%[23-24]。在作者系列研究中占11.3%,由于样本太少和辅助因子的数量较小,研究结果可能出现偏差。但在BORAIAH等[17]的研究中,同样发现Pauwels角对颈短缩无明显影响。体质量指数被认为是颈短缩的重要影响因素[20-21,23],但并未解释影响的原因。在一项Meta分析中发现,低体质量指数给骨折带来了相当重要的风险,这些骨折基本上独立于年龄和性别,但依赖于骨密度。作者认为,高体质量指数的患者在负重期间,股骨颈断端压缩力增大,骨折碎片沿内植物滑动距离增加,进而导致股骨颈短缩增加。
高龄与低骨密度被认为是颈短缩增加的危险因 素[17,19-20,25-27],实际上,这两个因素与骨密度之间的密切相关性并不难建立。 一般来说,随着年龄的增加,骨量的减少也会增加,这一结果影响了颈部缩短的发生率。在以往的研究中,对于骨密度的测量是通过Sing指数或T分来代 替[19,27],而SUNG等[14]建议用双能X射线吸收仪测量骨密度,结果颈短缩与骨密度无关,SUNG认为他们的研究更可靠,因为在研究中固定了骨折类型(嵌插型股骨颈骨折)与手术方式。THOMAS等[21]在研究非老年患者股骨颈骨折中发现,年龄与颈短缩无关,同样,在此次研究中,没有观察到与年龄的相关性。因此,作者假设,在骨质疏松发生率较低的非老年患者中,年龄与股骨颈缩短的相关性可能可以忽略不计。
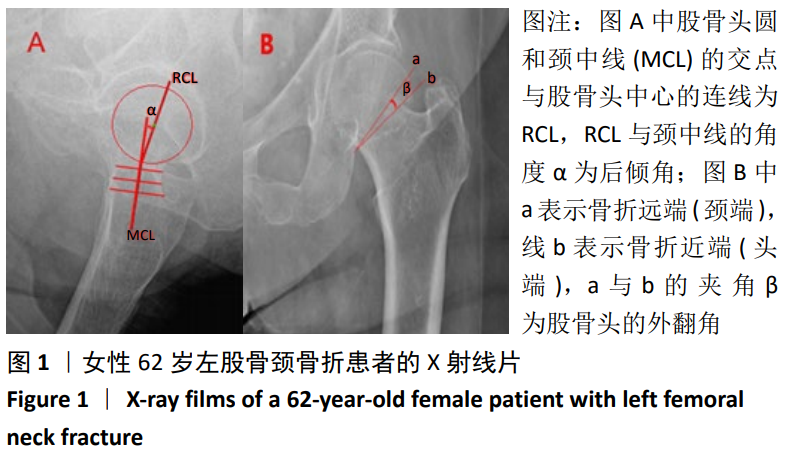
在现有文献对颈短缩影响因素的研究中,外翻角与后倾角很少被提及。为保证股骨头的血运及骨折固定的稳定性,在移位性股骨颈骨折中被要求解剖复位;而在嵌插型股骨颈骨折中,因骨折断端移位较小,嵌插较稳定,可以进行原位空心螺钉内固定[28],这导致股骨头有一定程度的外翻与后倾残留。在此次研究中,外翻角大小是预测嵌插型股骨颈骨折术后颈短缩的显著因子,这与SONG等[29]的研究结果一致,在他们的研究中,31-B1.1型骨折后颈短缩程度显著高于31-B1.2型(8.88 mm vs.3.70 mm)。
3.3 颈短缩的测量评价 对于股骨颈短缩程度的测量,文献中并无统一标准,大致包括以下几种类型:应用螺钉突出长度、股骨头塌陷程度、患肢短缩程度及关节-股骨转子间距的减少值来代替股骨颈短缩长度。SLOBOGEAN等[10]认为螺钉近端由于螺纹的把持较稳定,股骨颈短缩造成螺钉突出的变化发生在螺钉轨迹上,它反映了水平和垂直缩短的矢量和,但是忽略了未发生螺钉的凸出情况及由创伤或手术未能完全复位造成的颈短缩。ZLOWODZKI等[15]对最近一次拍摄的髋关节前后X射线片与受伤时拍摄的健侧髋关节X射线片进行了比较,这2张X射线片均被扫描,并使用图形软件将2张X射线片进行覆盖,并调整大小的差异,比较股骨颈在水平x(外展矩臂缩短)和垂直平面y(股骨长度减少)的缩短,并用螺钉直径的大小进行矫正。LIU等[19]将颈短缩的计算方法进行了改进,股骨颈的矢量短缩值z=ysin(θ)xcos(θ),θ代表颈干角。这两种方法都容易受到腿部旋转的明显影响。
在目前的研究中,由于图像处理软件能够放大图像、保存图片和调整不同胶片之间的差异,使用数字胶片和图像软件可能是测量颈缩短的理想方法。但这种类型的技术只有在适当的前瞻性计划下才有可能进行,以确保两个臀部都被成像,腿部旋转得到控制;而且对测量者对软件处理熟练度的要求较高。
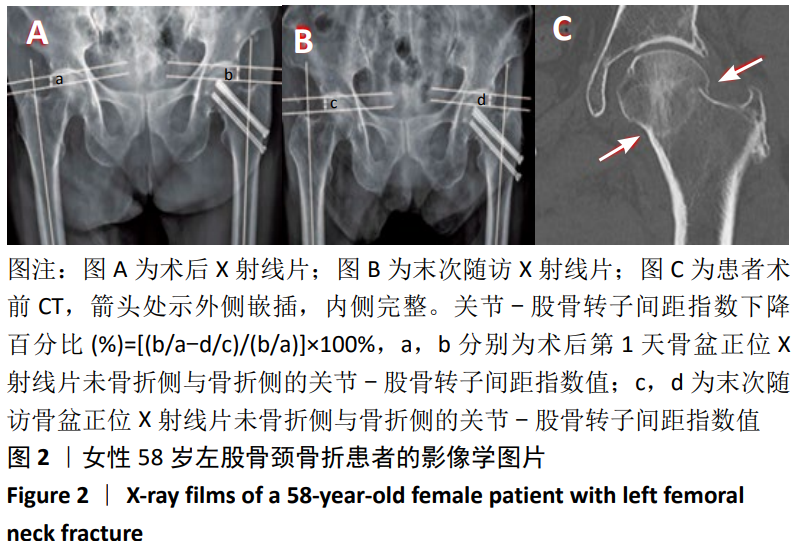
在此次研究中,采用YOON等[2]描述的利用关节-股骨转子间距指数下降百分比代替股骨颈短缩程度,这种方法可以排除股骨颈前倾、下肢旋转与外展对测量的影响;还可以通过放大图片进行测量,不需要按比例矫正,且不影响结果的准确性。这种方法操作较简单,对图像处理能力要求较低,缺点是不能测出颈短缩的具体数值。在后续的研究中,需要继续对这种测量方法进行评价与改进,明确关节-股骨转子间距指数下降百分比与颈短缩具体数值的换算过程。
3.4 颈短缩对功能的影响 在2007年ZLOWODZKI等[15]对骨科医师问卷调查发现颈短缩可能对功能造成负面影响之后[6],关于颈短缩对功能影响的研究不断开展。Zlowodzki等[15]在一项多中心队列的研究中发现,随着颈短缩的增加,患者SF-36量表平均物理功能评分从74分显著下降到53分,提示了梯度效应。同样,SLOBOGEAN等[10]在一些年轻股骨颈患者的病例中也发现严重颈缩短与临床上重要的功能下降有关。在BORAIAH等[17]的研究中,造成功能显著下降的颈短缩长度分别为5 mm与10 mm。CROSBY等[30]分析了519例平均年龄为76岁的患者,发现股骨颈塌陷大于 15 mm与残余疼痛增加有关。BORAIAH等[17]发现外展矩臂的减少对SF-36量表中的身体疼痛评分有明显的影响。此外,RACZKOWSKI 等[31]报道颈短缩和伴随的腿长差异是已知的膝关节、髋关节和脊柱骨关节炎的诱发因素,最终导致疼痛和残疾。
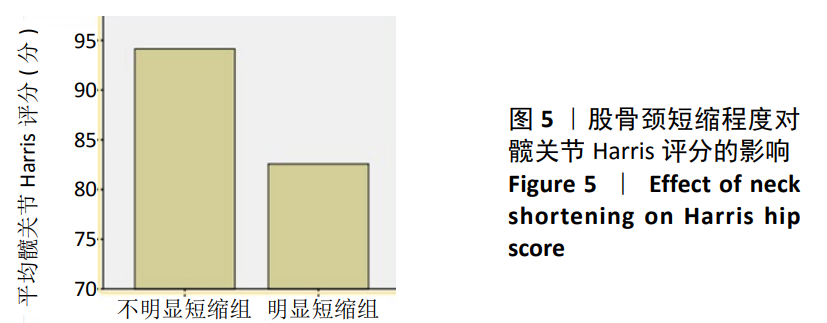
在此次研究中,明显短缩组和不明显短缩组的髋关节Harris评分分别为(82.57±5.12)分和(94.15±4.03)分,差异有显著性意义(t=6.842,P < 0.05)。短缩患者主要表现为疼痛(如久坐、站立及长距离步行后疼痛)与跛行,在以往研究对这一结果的解释如下:①髋关节外展肌主要有臀中肌和臀小肌,这两块肌肉附着于大转子上,股骨颈短缩的增加导致髋关节外展肌矩臂的减少,外展肌的作用是抵消由体质量引起的中央垂直力,从而在行走过程中的单腿姿势阶段稳定骨盆,外展矩臂的减少增加了行走所需的外展力以及关节反应力,外展结构的故障可能导致跛行[12]。②双下肢腿长差异导致跛行,ZIELINSKI等[20]认为适当地增高足跟高度(即使用增高鞋垫等)可以缓解跛行症状,他们还提出将步态速度作为评价功能的一项指标。此外,手术、术后固定和疼痛也可能导致异常或不对称的步态模式和肌力下降。③物理功能下降另一个可能的解释是由于螺钉后退而引起的局部刺激,导致疼痛与异物感。如果骨折非解剖复位,股骨头和髋臼之间的错位可能会损害功能;如果不能恢复头部和髋臼之间的适当关系,可能会对结果产生负面影响[15]。
在作者的后续随访中,发现内植物取出可以改善髋关节功能(尤其是明显短缩的患者),平均增加值为4分(-2-8分);在明显短缩组有5例患者取出内固定,Harris评分增加值为4-8分,患者疼痛症状减轻或消失;但也有2例患者内固定取出后髋关节Harris评分轻微降低。对于内固定是否应该去除,暂无定论。MINKOWIJZ等[32]认为对于骨折固定手术区域疼痛,在排除其他原因导致疼痛(如感染和不愈合)的情况下,去除内植物是安全、风险最小的疼痛缓解和功能改善方法。对于髋关节Harris评分降低的情况,作者的解释是在去除内固定的手术中,与第一次微创手术相比,扩大切开,造成组织损伤与瘢痕粘连;作者认为,在患者要求取出内植物时,医师应该评估患者术后功能情况,避免术后功能降低。
此次研究的局限性如下:它是一个回顾性的设计,有选择偏差;病例数较少,明显短缩组仅有7例,容易夸大研究结果;在X射线平片上测量股骨头外翻及后倾角较困难,容易增加测量误差。
3.5 结论 股骨头外翻程度是65岁以下嵌插型股骨颈骨折术后颈短缩的显著预测因子,随着颈短缩的增加,髋关节功能降低;对于螺钉凸出造成的髋部疼痛,内植物取出可以有效改善这种症状。总之,骨科医师在临床工作中,不应以骨愈合作为手术成功的唯一标准,还要更多地关注患者术后的功能恢复情况。
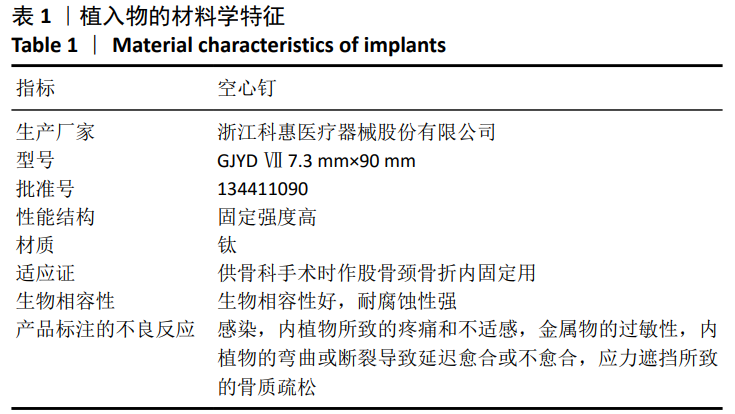
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程