[1] SLOAN M, PREMKUMAR A, SNETH NP. Projected volume of primary total joint arthroplasty in the US, 2014 to 2030. JBJS. 2018;100(17): 1455-1460.
[2] GANDHI R, PETRUCCELLI D, DEVEREAUX PJ, et al. Incidence and timing of myocardial infarction after total joint arthroplasty. J Arthroplasty. 2006;21(6): 874-877.
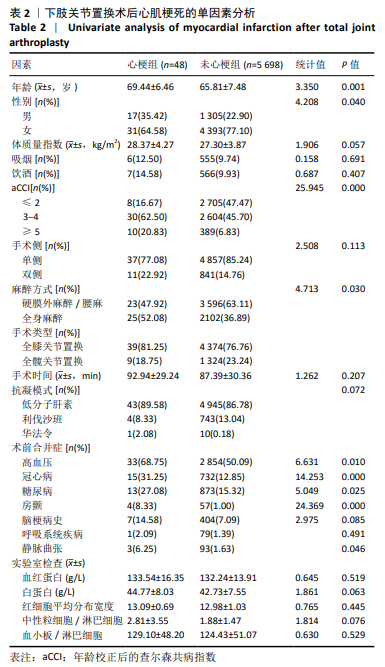
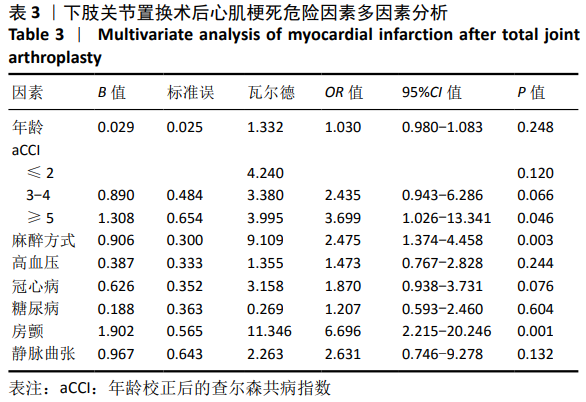
[3] MENENDEZ ME, MEMTSOUDIS SG, OPPERER M, et al. A nationwide analysis of risk factors for in-hospital myocardial infarction after total joint arthroplasty. Int Orthop. 2015;39(4):777-786.
[4] 王腾科,高洁. 老年患者单侧膝关节置换术后急性心肌梗死危险因素分析[C].proceedings of the 中国中西医结合麻醉学会[CSIA]年会暨第二届全国中西医结合麻醉学术研讨会、江苏省中西医结合学会麻醉专业委员会成立大会, F, 2015
[5] 徐饶,荆鑫,陆鸣,等.术前心血管危险因素对人工关节置换术并发症的影响分析[J].中外医学研究,2015,13(33): 33-35.
[6] CHARLSON M, SZATROWSKI TP, PETERSON J, et al. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245-1251.
[7] IASONOS A, SCHRAG D, RAJ GV, et al. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008;26(8):1364-1370.
[8] WILSON JM, FARLEY KX, ERENS GA, et al. General vs spinal anesthesia for revision total knee arthroplasty: do complication rates differ?. J Arthroplasty.2019;34(7):1417-1422.
[9] CHI D, MARIANO ER, MEMTSOUDIS SG, et al. Regional Anesthesia and Readmission Rates After Total Knee Arthroplasty. Anesth Analg. 2019;128(6):1319-1327.
[10] STAMBOUGH JB, BLOOM GB, EDWARDS PK, et al. Rapid recovery after total joint arthroplasty using general anesthesia. J Arthroplasty. 2019; 34(9):1889-1896.
[11] PUGELY AJ, MARTIN CT, GAO Y, et al. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. JBJS.2013;95(3):193-199.
[12] BAUQUES BA, TOY JO, BOHL DD, et al. General compared with spinal anesthesia for total hip arthroplasty . J Bone Joint Surg Am. 2015;97(6): 455.
[13] 程浩,郭恩琪. 比较全身麻醉和椎管内麻醉在全髋关节置换术中的临床应用价值[J].中华全科医学, 2016,14(5):724-726.
[14] 吴继敏,樊理华,章玲宾,等.硬膜外麻醉与全身麻醉在膝关节置换术中的应用[J].中国乡村医药, 2013,20(22):44-45.
[15] WEDI E, VON RENTELN D, GONZALEZ S, et al. Use of the over-the-scope-clip (OTSC) in non-variceal upper gastrointestinal bleeding in patients with severe cardiovascular comorbidities: a retrospective study. Endosc Int Open. 2017;5(9):E875-E882.
[16] AGGARWAL VK, TISCHLER EH, POST ZD, et al. Patients with atrial fibrillation undergoing total joint arthroplasty increase hospital burden. JBJS.2013;95(17):1606-1611.
[17] JIANG T, SONG K, YAO Y, et al. Perioperative allogenic blood transfusion increases the incidence of postoperative deep vein thrombosis in total knee and hip arthroplasty. J Orthop Surg Res.2019;14(1):235.
[18] HU C, LIU C, WANG Y, et al. The Timing of Symptomatic Pulmonary Embolism in Patients With Nonwarfarin Anticoagulants Following Elective Primary Total Joint Arthroplasty. J Arthroplasty. 2020;35(6): 1703-1707.
[19] MORELLA P, SACCO M, CARAFA M, et al. Permanent atrial fibrillation and pulmonary embolism in elderly patients without deep vein thrombosis: is there a relationship? Aging Clin Exp Res. 2019; 31(8): 1121-1128.
[20] LEE S, HWANG JI, KIM Y, et al. Venous Thromboembolism Following Hip and Knee Replacement Arthroplasty in Korea: A Nationwide Study Based on Claims Registry.J Korean Med Sci.2016;31:80-88.
[21] PARVIZI J, HUANG R, RAPHAEL IJ, et al. Symptomatic pulmonary embolus after joint arthroplasty: stratification of risk factors. Clin Orthop Relat Res. 2014;472(3):903-912.
[22] CHARLSON ME, POMPEI P, ALES KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383.
[23] SCHMOLDERS J, FRIEDRICH MJ, MICHEL R, et al. Validation of the Charlson comorbidity index in patients undergoing revision total hip arthroplasty. Int Orthop.2015;39(9):1771-1777.
[24] VOSKUIJL T, HAGEMAN M, RING D. Higher Charlson Comorbidity Index Scores are Associated With Readmission After Orthopaedic Surgery. Clin Orthop Relat Res. 2013;472(5):1638.
[25] SOOHOO NF, FARNG E, LIEBERMAN JR, et al. Factors that predict short-term complication rates after total hip arthroplasty. Clin Orthop Relat Res. 2010;468(9):2363-2371.
[26] NUZHAT N, ANAYA M, DE QUEIROZ CAMPOS G, et al. Characterizing Comorbidities in Total Joint Arthroplasty Patients in a Safety-Net Hospital Using the Age-Adjusted Charlson Comorbidity Index. J Orthop Exp Innovat. 2020;1(1):12159.
[27] MARYA SKS, AMIT P, SINGH C. Impact of Charlson indices and comorbid conditions on complication risk in bilateral simultaneous total knee arthroplasty. Knee.2016;23(6):955-959.
[28] WUERZ TH, KENT DM, MALCHAU H, et al. A nomogram to predict major complications after hip and knee arthroplasty. J Arthroplasty. 2014;29(7):1457-1462.
[29] BABAZADE R, SREENIVASALU T, JAIN P, et al. A nomogram for predicting the need for sciatic nerve block after total knee arthroplasty. J Anesth. 2016;30(5):864-872.
[30] GRONBECK C, COTE MP, HALAWI MJ. Predicting inpatient status after primary total knee arthroplasty in Medicare-aged patients. J Arthroplasty. 2019;34(7):1322-1327.
[31] MESKO NW, BACHMANN KR, KOVACEVIC D, et al. Thirty-day readmission following total hip and knee arthroplasty–a preliminary single institution predictive model. J Arthroplasty. 2014;29(8): 1532-1538.
[32] 张华, 陶立元, 赵一鸣.开展病历回顾性研究的注意事项[J].中华儿科杂志,2018, 56(1):47. |