中国组织工程研究 ›› 2020, Vol. 24 ›› Issue (9): 1318-1323.doi: 10.3969/j.issn.2095-4344.2469
• 人工假体 artificial prosthesis • 上一篇 下一篇
直接前侧入路与前外侧入路全髋关节置换的差异:基于置换后早期患者主观感受的比较
米尔阿里木·木尔提扎1,赵 巍1,瓦热斯江·尼牙孜2,袁 宏1,王 利1
- 新疆维吾尔自治区人民医院骨科中心,1骨科关节与老年骨病病区,2脊柱二病区,新疆维吾尔自治区乌鲁木齐市 830001
Direct anterior approach versus anterolateral approach in total hip arthroplasty: comparison of early postoperative patient’s perception
Milalimmu·Multiza1, Zhao Wei1, Varesjiang·Nyyaz2, Yuan Hong1, Wang Li1
- 1Department of Orthopedic Joint and Geriatric Osteopathy, 2Second Department of Spine, Orthopedic Center, Xinjiang Uygur Autonomous Region People’s Hospital, Urumqi 830001, Xinjiang Uygur Autonomous Region, China
摘要:
文题释义:
直接前方入路:能够较好的保护髋关节周围肌肉及软组织,由传统的Smith-Peterson入路改良,经阔筋膜张肌与缝匠肌间隙,故经过此入路行人工髋关节置换术后,能够使关节更加稳定,术后脱位率更低。但是该手术入路学习曲线较长,术中需要具备一定的经验,且对手术室硬件条件有相应的要求。
牛津髋关节功能评分:该系统是由6项疼痛相关和6项日常活动(如行走、穿衣服、睡觉等)内容组成,自2007年修改后,被广泛应用于骨关节外科领域。该系统更加客观易懂,更能有效量化患者主观感受,故在实际临床随访中能够更好的执行及随访。
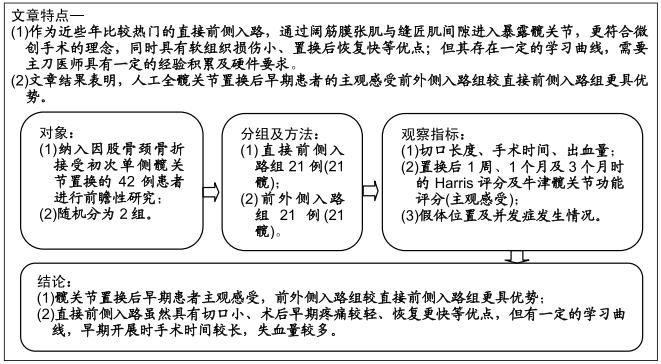
背景:人工全髋关节置换能够显著缓解终晚期髋关节疾病患者疼痛,有效改善其关节功能。不同手术入路各有其优势及不足。作为近些年比较热门的直接前侧入路,通过阔筋膜张肌与缝匠肌间隙进入暴露髋关节,更符合微创手术的理念,同时具有软组织损伤小、置换后恢复快等优点;但其存在一定的学习曲线,需要主刀医师具有一定的经验积累及硬件要求。
目的:基于置换后早期患者主观感受比较直接前侧入路及前外侧入路行人工全髋关节置换治疗老龄单侧股骨颈骨折的差异。
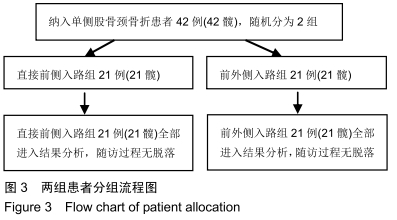
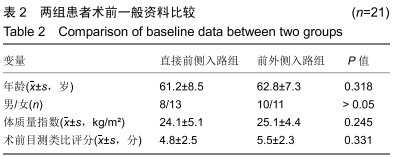
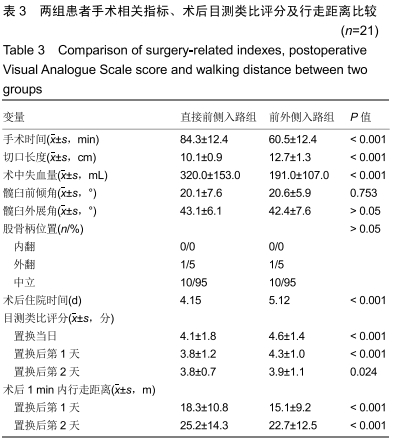
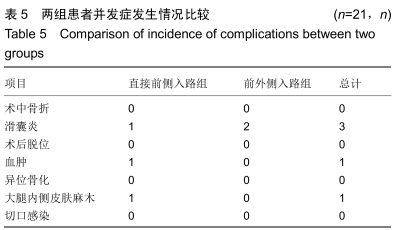
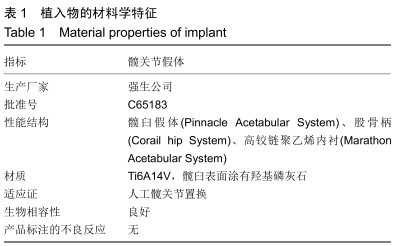
方法:纳入2017年1月至2018年6月新疆维吾尔自治区人民医院骨科中心收治的单侧股骨颈骨折患者42例(42髋),均接受人工髋关节置换治疗。随机分为2组,直接前侧入路组21例患者(21髋),前外侧入路组21例患者(21髋)。2组患者对治疗方案均知情同意,且得到医院伦理委员会批准。记录2组患者的手术切口长度、手术时间、出血量;对比2组患者术后1周、1个月及3个月时的髋关节Harris评分及主观牛津髋关节功能评分;并观察假体位置及并发症情况。
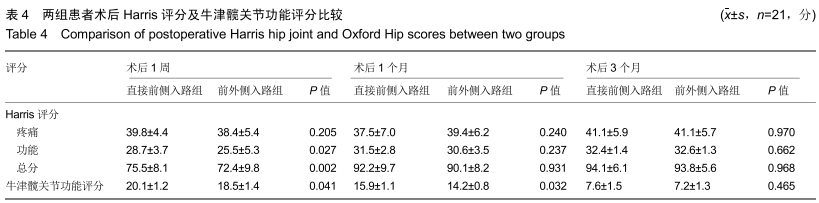
结果与结论:①直接前侧入路组患者较前外侧入路组患者术后出院时间更早(P < 0.001);手术切口长度直接前侧入路组小于前外侧入路组(P < 0.001);手术时间及术中出血比较,直接前侧入路组大于前外侧入路组 (P < 0.001);②术后第1,2天,直接前侧入路组患者1 min内行走距离均大于前外侧入路组(P < 0.001),疼痛目测类比评分低于前外侧入路组(P < 0.05);③术后3个月随访时,2组患者髋臼假体外展角及前倾角差异均无显著性意义(P > 0.05);④术后1周时Harris评分及主观牛津髋关节功能评分比较,直接前侧入路组均高于前外侧入路组(P < 0.05);术后3个月髋关节Harris评分及牛津髋关节功能评分2组差异无显著性意义(P > 0.05);⑤直接前侧入路组1例、前外侧入路组2例患者切口周围出现滑囊炎,患者感疼痛不适,经局部封闭注射后,症状均消失;1例直接前侧入路组患者术后出现切口血肿,术后3周时自愈;1例直接前侧入路组患者术后出现大腿切口内侧缘皮肤感觉麻木;⑥结果表明,人工全髋关节置换后早期患者主观感受前外侧入路组较直接前侧入路组更具优势。直接前侧入路虽然具有切口小、术后早期疼痛较轻、恢复更快等优点,但有一定的学习曲线,早期开展时手术时间较长,失血量较多。
ORCID: 0000-0003-1981-7259(米尔阿里木·木尔提扎)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号: