中国组织工程研究 ›› 2021, Vol. 25 ›› Issue (21): 3409-3415.doi: 10.3969/j.issn.2095-4344.3851
• 骨与关节循证医学 evidence-based medicine of the bone and joint • 上一篇 下一篇
全髋关节置换中前外侧微创入路与后外侧入路疗效差异的Meta分析
付攀峰,商 炜,亢 哲,邓 宇,祝少博
- 武汉大学中南医院骨科,湖北省武汉市 430071
Efficacy of anterolateral minimally invasive approach versus traditional posterolateral approach in total hip arthroplasty: a meta-analysis
Fu Panfeng, Shang Wei, Kang Zhe, Deng Yu, Zhu Shaobo
- Department of Orthopedic Surgery, Zhongnan Hospital, Wuhan University, Wuhan 430071, Hubei Province, China
摘要:
文题释义:
全髋关节置换:是以人工合成的髋关节假体代替已损坏的股骨头和髋臼,以恢复髋关节的活动和负重功能的一种修复方式。
阔筋膜张肌:位于大腿上部前外侧,起自髂前上棘,肌腹被包在阔筋膜的两层之间,向下移行为髂胫束,止于胫骨外侧髁。
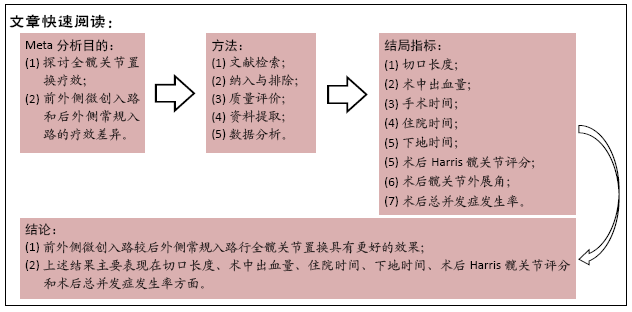
目的:全髋关节置换采用前外侧微创入路相比后外侧常规入路具备某些优势,但其是否具有和后外侧常规入路一样的良好疗效尚存争议。文章应用Meta分析评价前外侧微创入路与后外侧常规入路行全髋关节置换的临床疗效差异。
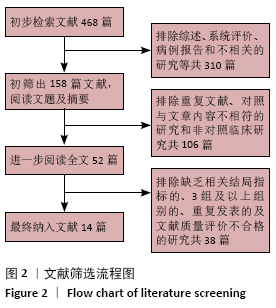
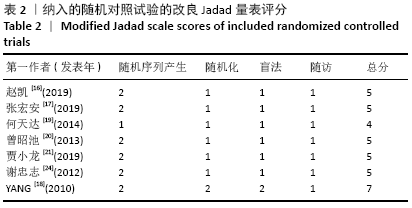
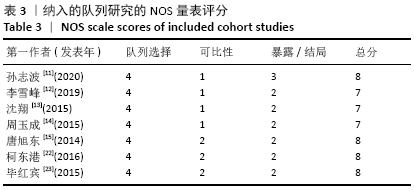
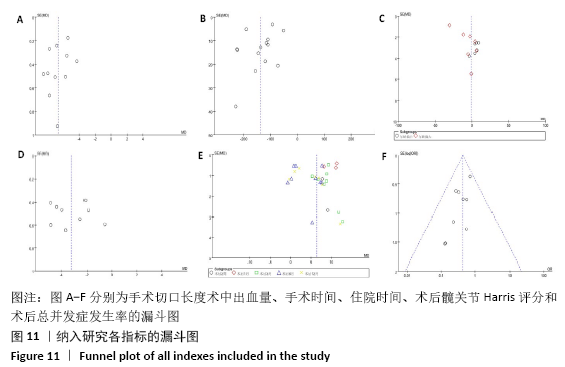
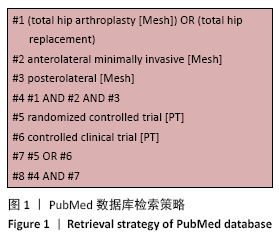
方法:计算机检索英文数据库PubMed、Embase、The Cochrane Library、Web of Science,以及中文数据库中国知网、维普、万方和CBM数据库,检索时间为建库至2020年6月,按照既定纳入排除标准筛选已发表的临床对照研究,严格评价文献质量并提取数据,采用RevMan 5.3软件进行结果数据分析。
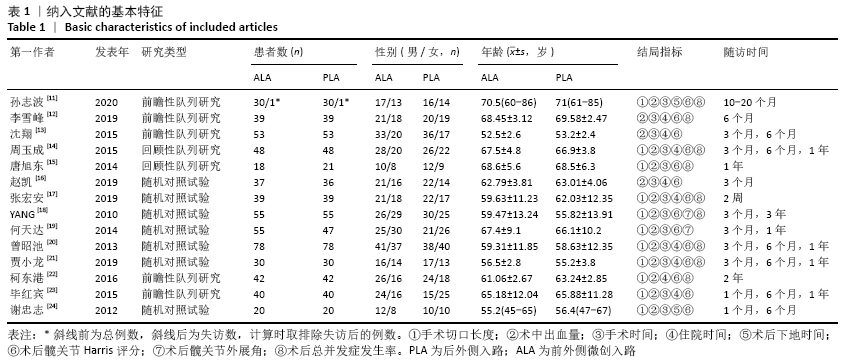
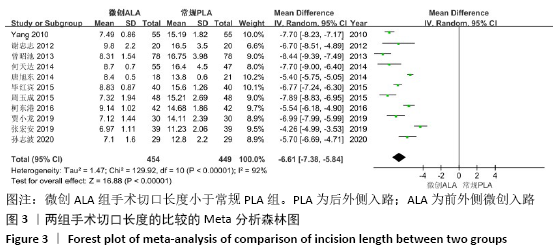
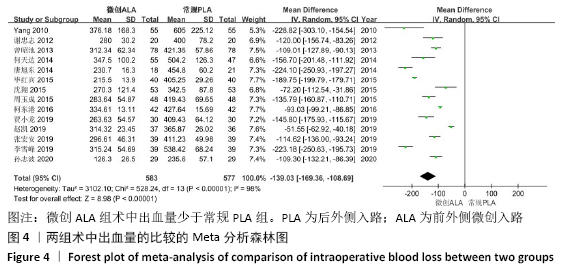
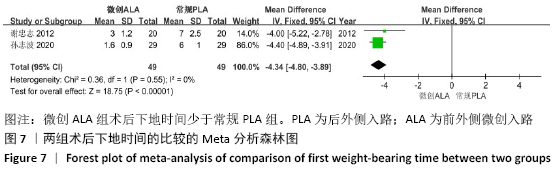
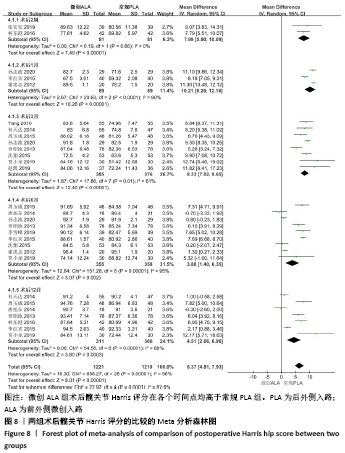
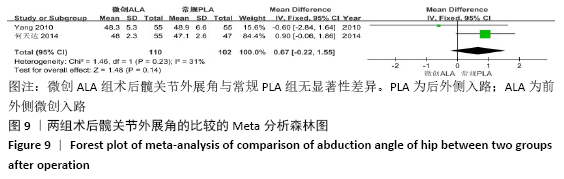
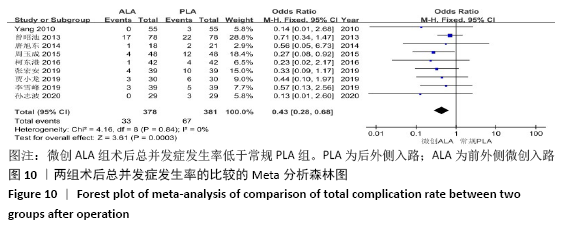
结果:①共纳入14篇文献,纳入患者1 160例,其中包括7项随机对照试验和7项队列研究,均为高质量研究;②Meta分析结果显示,前外侧微创入路比后外侧常规入路切口长度小(MD=-6.61,95%CI:-7.38至-5.84,P < 0.000 01),术中出血量少(MD=-139.03,95%CI:-169.36至-108.69,P < 0.000 01),住院时间短(MD=-3.19,95%CI:-4.14至-2.24,P < 0.000 01),下地时间早(MD=-4.34,95%CI:-4.80至-3.89,P < 0.000 01),术后各时间点Harris髋关节功能评分高(MD=6.37,95%CI:4.81-7.93,P < 0.000 01),总并发症发生率低(OR=0.43,95%CI:0.28-0.68,P=0.000 3),而手术时间(MD=-1.12,95%CI:-11.03-8.78,P=0.82)与髋关节外展角(MD=0.67,95%CI:-0.22-1.55,P=0.14)无显著差异。
结论:前外侧微创入路较后外侧常规入路行全髋关节置换具有更好的效果,能更好地保证手术的安全性和有效性,减少并发症,促进术后髋关节功能恢复,是更具优势的手术入路方式,而更多的评价指标如术后疼痛评分、住院费用和术后髋关节脱位率等尚需未来进一步研究分析验证。
https://orcid.org/0000-0002-8334-4524 (付攀峰)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号: