中国组织工程研究 ›› 2014, Vol. 18 ›› Issue (48): 7855-7861.doi: 10.3969/j.issn.2095-4344.2014.48.026
• 骨与关节循证医学 evidence-based medicine of the bone and joint • 上一篇 下一篇
后外侧融合与椎间融合修复成人腰椎滑脱的Meta分析
阿忍别克•哈布力汗,金格勒,李忠伟,努尔哈那提•纱衣兰别克
- 新疆医科大学第一附属医院骨科,新疆维吾尔自治区乌鲁木齐市 830054
Posterolateral fusion and interbody fusion in repair of adult lumbar spondylolisthesis: a meta-analysis
Arenbieke•Habulihan, Jin Ge-le, Li Zhong-wei, Nuerhanati•Shayilanbieke
- Department of Orthopedics, the First Affiliated Hospital of Xinjiang Medical University, Urumqi 830054, Xinjiang Uygur Autonomous Region, China
摘要:
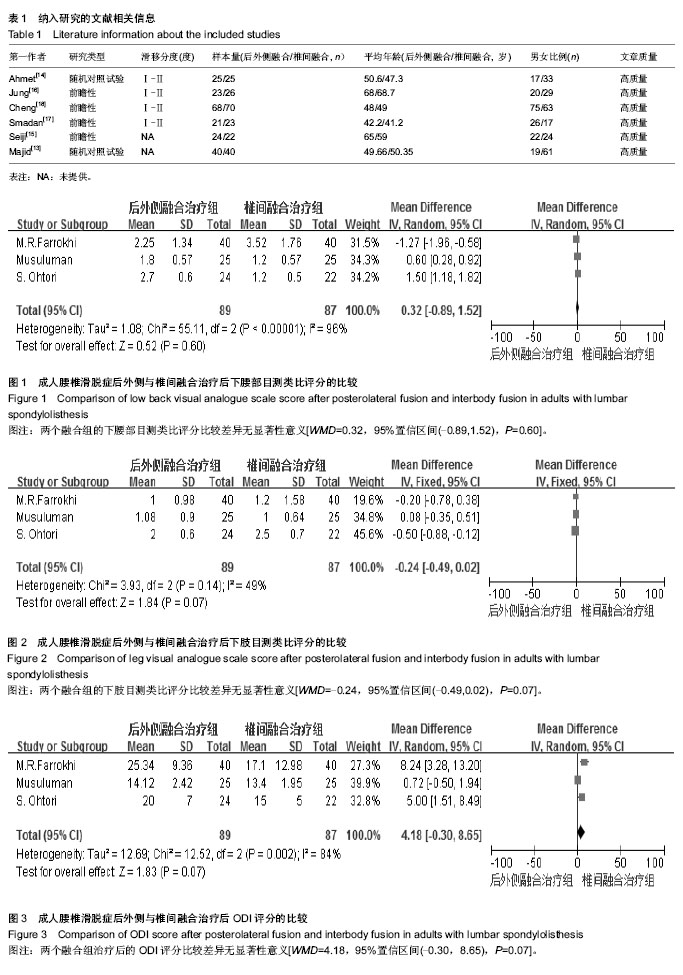
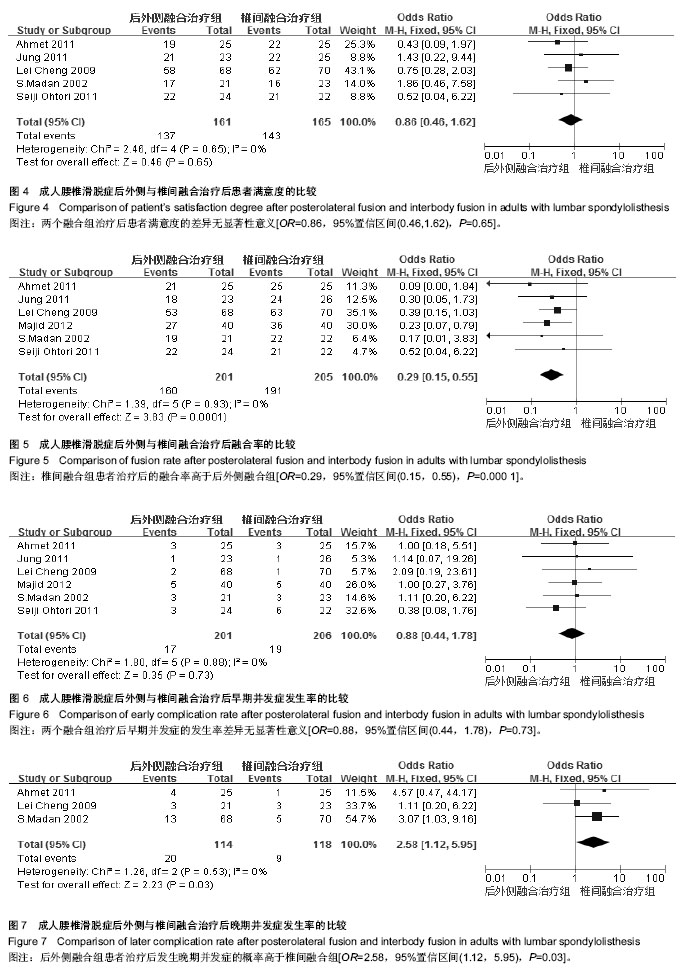
背景:融合治疗是腰椎滑脱症手术中必不可少的重要部分。融合的主要目的是椎间关节之间发生骨性结合,从建立和维持比较坚强脊柱稳定性。腰椎滑脱症常用的融合方式为后外侧融合与椎间融合。虽然上述两种融合方式治疗后具有临床疗效良好以及并发症发生率较低等优势,但在临床上对于腰椎滑脱的最佳融合方式仍存争议。 目的:对后外侧融合与椎间融合修复成人腰椎滑脱症的疗效进行评价。 方法:按照Cochrane系统评价的方法,计算机检索Medline(2000年至2014年3月)、PubMed(2000年至2014年3月)、Springerlink(2000年至2014年3月),并采用手工检索等方法收集文献。文献检索语言只限制为英文。收集所有相关的随机对照研究和高质量队列研究,采用Cochrane协作网提供的软件Revmen 5.2.0进行Meta分析,以获得后外侧融合与椎间融合治疗成人腰椎滑脱症的临床疗效及影像学疗效相关的文献。 结果与结论:经全面检索及筛查后,共纳入2篇高质量随机对照研究、4篇高质量队列研究进行评价。Meta分析结果显示,后外侧融合与椎间融合患者治疗后下腰部末次目测类比评分[WMD=0.32,95%置信区间(-0.89,1.52),P=0.60]、下肢末次目测类比评分[WMD=-0.24,95%置信区间(-0.49,0.02),P=0.07]、腰痛ODI评分[WMD=4.18,95%置信区间(-0.30, 8.65),P=0.07]、治疗后满意率[OR=0.86,95%置信区间(0.46,1.62),P=0.65]和治疗后早期并发症发生率[OR=0.88,95%置信区间(0.44,1.78),P=0.73]差异无显著性意义,疗效基本相同。椎间融合组的融合率明显高于后外侧融合组[OR=0.29,95%置信区间(0.15,0.55), P=0.000 1];后外侧融合组的晚期并发症发生率高于椎间融合组[OR=2.58,95%置信区间(1.12,5.95),P=0.03]。两个融合组患者治疗后下腰部及下肢疼痛和功能恢复情况相比治疗前均有明显改善。提示椎间融合组的融合率明显高于后外侧融合组,后外侧融合治疗会有更高的远期并发症发生率,研究包含的其余疗效指标两个融合治疗组之间无明显差别。
中图分类号: