中国组织工程研究 ›› 2019, Vol. 23 ›› Issue (16): 2500-2505.doi: 10.3969/j.issn.2095-4344.1206
• 骨科植入物 orthopedic implant • 上一篇 下一篇
锁定钢板及锁定螺钉内固定治疗Sanders Ⅲ型跟骨骨折:改良“L”型切口植骨与“L”型切口非植骨1年随访比较
孔长庚,郭 祥,吴多庆
- 中南大学湘雅医学院附属海口医院骨科,海南省海口市 570208
Internal fixation with locking plate and nail for treating Sanders III calcaneal fractures: one-year follow-up of modified “L-shape” incislon and bone graft versus “L-shape” incision without bone gratft
Kong Changgeng, Guo Xiang, Wu Duoqing
- Department of Orthopedics, Central South University Xiangya School of Medicine Affiliated Haikou Hospital, Haikou 570208, Hainan Province, China
摘要:
文章快速阅读:
.jpg)
文题释义:
Sanders 分型:根据跟骨骨折片段的数目、位置、冠状位及轴位CT检查结果进行分类。跟骨后关节面由平行于跟骨纵轴的 A、B两线分为3个等大域区,即内侧、中央和外侧柱,第3条骨折线C与后面的内侧边界一致,并同载距突分开,由此产生4个潜在的骨折片段,骨折线由外向内用 A、B、C 标明。Ⅰ型:所有无移位的关节内骨折,不论后关节面骨折线的多少;Ⅱ型:后关节面2片段骨折,根据原发骨折线的位置又分为ⅡA 型、ⅡB 型及ⅡC型3个亚型;Ⅲ型:后关节面3片段骨折,按照2个骨折线的位置分为ⅢAB 型、ⅢAC 型和ⅢBC型3个亚型;Ⅳ型:后关节面4片段以上骨折,为严重粉碎性关节内骨折。
Böhler角(跟骨结节关节角):由跟骨结节与跟骨后关节突的连线与跟骨前-后关节突连接形成的夹角,正常值为25°-40°。Böhler角的恢复是判断跟骨骨折预后功能良好与否的主要因素。测量方法:跟骨侧位X射线平片,作跟骨结节上缘至跟距关节后关节面上缘的连线,再作跟骰关节上缘与跟距关节后关节面的切线,两线相交的锐角为跟骨结节关节角。
Gissane角(跟骨交叉角):是指跟距关节前后关节面之间的夹角,正常值为120°-145°。Gissane角是判断跟骨骨折损伤程度和评估跟骨骨折治疗疗效指标之一,测量方法:跟骨侧位X射线平片,以跟骨沟分别连接跟骨前突和跟骨后突关节面上缘连线的交角。
摘要
背景:目前临床上跟骨复杂关节内骨折以切开复位内固定为主要治疗方案,但传统“L”型切口相关并发症仍较高,术中植骨与否仍存在较大争议,因此选择合适的修复方案提高临床疗效的同时降低术后并发症一直是国内外学者研究的热点。
目的:探讨改良“L”型切口植骨内固定治疗Sanders Ⅲ型跟骨骨折的临床效果。
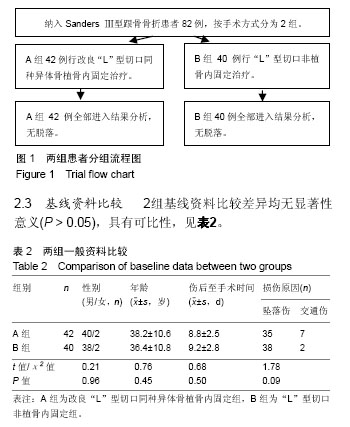
方法:回顾性分析进行手术治疗获得1年以上随访的单侧新鲜Sanders Ⅲ型跟骨骨折患者82例,分为2组,改良“L”型切口植骨组42例(A组),“L”型切口非植骨组40例(B组)。比较2组患者手术时间、切口愈合时间、住院时间、负重时间、足部功能、并发症发生率及手术前后影像学参数。
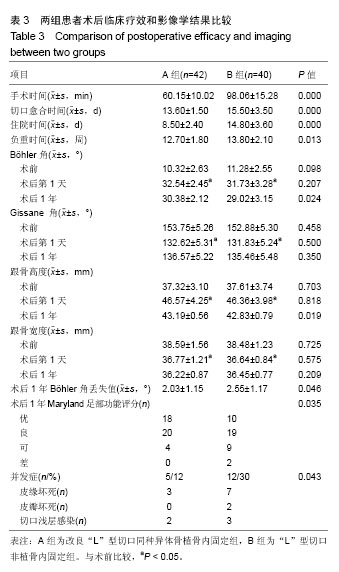
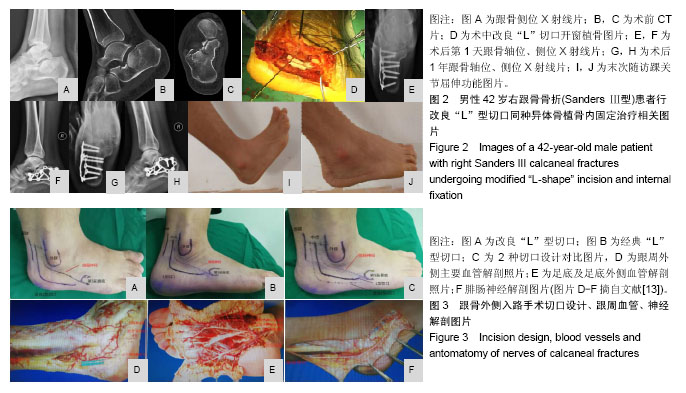
结果与结论:①A组患者的手术时间、切口愈合时间、住院时间及负重时间均短于B组(P < 0.05);②术后2组跟骨Böhler角、Gissane角、跟骨宽度、高度恢复差异无显著性意义(P > 0.05);③术后1年随访时,2组Gissane角、跟骨宽度差异无显著性意义(P > 0.05);但Böhler角及跟骨高度差异有显著性意义,A组大于B组(P < 0.05);且2组均出现Böhler角丢失现象,A组Böhler角丢失值明显低于B组(P < 0.05);④A组Maryland足功能评分及优良率均优于B组,差异有显著性意义(P < 0.05);⑤A组切口并发症发生率明显低于B组(12% vs. 30%),差异有显著性意义(P < 0.05);⑥提示改良“L”型切口植骨内固定治疗Sanders Ⅲ型跟骨骨折可获得良好的复位,术后切口并发症少,植骨可减少术后Bohler角丢失,获得满意的临床疗效。
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
ORCID: 0000-0002-4364-3175(孔长庚)
中图分类号:
.jpg)
.jpg)