中国组织工程研究 ›› 2019, Vol. 23 ›› Issue (4): 573-577.doi: 10.3969/j.issn.2095-4344.1039
• 数字化骨科 digital orthopedics • 上一篇 下一篇
腰骶丛神经根的应用解剖及临床意义
朱爱国1,张 烽2,朱建炜2,金国华3
- 1江苏省如东县人民医院骨科,江苏省如东县 226400;2南通大学附属医院骨科,江苏省南通市 226001;3南通大学医学院解剖学教研室,江苏省南通市 226001
Anatomic measurement and clinical significance of the lumbosacral nerve roots
Zhu Aiguo1, Zhang Feng2, Zhu Jianwei2, Jin Guohua3
- 1Department of Orthopedics, Rudong People’s Hospital,Rudong 226400, Jiangsu Province, China; 2Department of Orthopedics, Affiliated Hospital of Nantong University, Nantong 226001, Jiangsu Province, China; 3Department of Anatomy, Medical School of Nantong University, Nantong 226001, Jiangsu Province, China
摘要:
文章快速阅读:
.jpg)
文题释义:
腰骶丛:由腰丛和骶丛组成。腰丛来源于L1-3神经根前支、一部分T12和一部分L4,其位于腰大肌深面、腰椎横突前方。腰丛的主要分支为股神经(L2-4后股)、闭孔神经(L2~4前股),还包括支配腰大肌、髂肌和腰方肌的肌支和股前外侧皮神经(L2-3)、髂腹下神经(L1)、髂腹股沟神经(L1)、生殖股神经(L1-2)。骶丛来源于L4-5、S1-3神经根前支和一部分S4前支,其中L4-5神经根组成腰骶干。
硬膜囊:处在脊椎尾端所有神经汇聚的地方,是保护脊髓的一种组织,在S2水平由硬脊膜和蛛网膜封闭而成,包绕中枢神经系统外的一层硬膜(分为硬脊膜和硬脑膜),硬膜所构成的囊状结构称为硬膜囊。
摘要
背景:后入路行下腰椎体次全切除重建可损伤腰骶丛神经。
目的:观测腰骶丛神经根间距离和对应腰椎体冠状截面的大小关系,为后入路行下腰椎体次全切除重建的安全性提供解剖学依据。
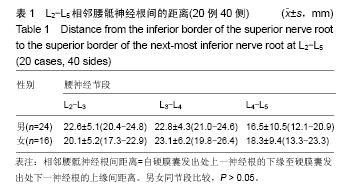
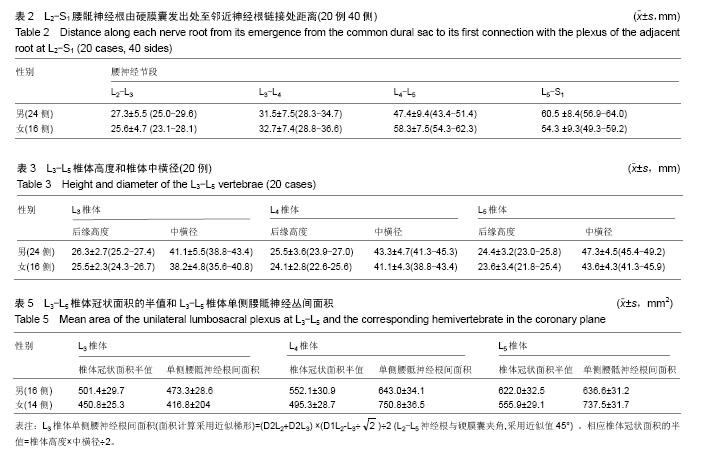
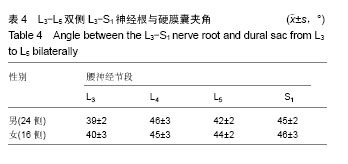
方法:解剖20具成人尸体的双侧腰骶丛和对应腰椎椎体,观察腰骶丛神经的走行特点。测量双侧L2-L5相邻腰神经根自硬膜囊发出处之间距离、双侧L2-L5腰神经根由硬膜囊发出处至邻近神经根链接处距离;测量L3-L5椎体高度和中横径长度;测量双侧L3-L5脊神经神经根与硬膜囊夹角。
结果与结论:①L3椎体单侧腰骶丛间面积平均值较对应椎体冠状面积半值平均值小30 mm2左右;②L4椎体单侧腰骶丛间面积平均值较对应椎体冠状面积半值平均值大100-150 mm2;③L5椎体单侧腰骶丛神经间面积平均值较对应椎体冠状面积半值平均值男性大15 mm2,女性大180 mm2;④后入路次全切除L3,L4,L5椎体并重建时腰骶丛神经根无解剖上的危险,而次全切除L4安全性最高。
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
ORCID: 0000-0002-1631-9011(朱爱国)
中图分类号:
.jpg)
.jpg)