[1] ZHAO DW, HU YC. Chinese experts’ consensus on the diagnosis and treatment of osteonecrosis of the femoral head in adults. Orthop Surg. 2012;4(3):125-130.
[2] ZHAO D, ZHANG F, WANG B, et al. Guidelines for clinical diagnosis and treatment of osteonecrosis of the femoral head in adults (2019 version). J Orthop Translat. 2020;21: 100-110.
[3] KANG JS, MOON KH, KWON DG, et al. The natural history of asymptomatic osteonecrosis of the femoral head. Int Orthop. 2013;37(3):379-384.
[4] 韩杰,林智宇,徐志为,等. miRNA通过骨代谢机制干预股骨头坏死[J]. 中国组织工程研究,2023,27(32):5238-5248.
[5] SCHUR MD, LEE C, ARKADER A, et al. Risk factors for avascular necrosis after closed reduction for developmental dysplasia of the hip. J Child Orthop. 2016;10(3):185-192.
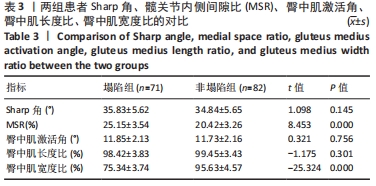
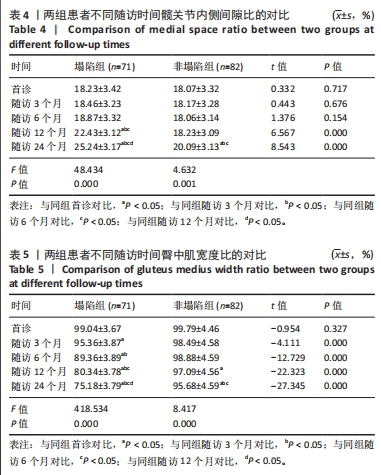
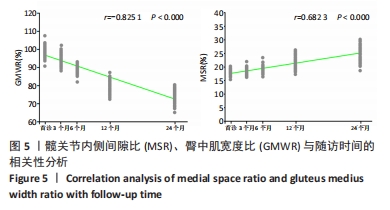
[6] LIN T, LI K, CHEN W, et al. Relationship between hip joint medial space ratio and collapse of femoral head in non-traumatic osteonecrosis: a retrospective study. J Hip Preserv Surg. 2021;8(4):311-317.
[7] 中国成人股骨头坏死临床诊疗指南(2020)[J]. 中华骨科杂志,2020,40(20):1365-1376.
[8] MEIER R, KRAUS TM, SCHAEFFELER C, et al. Bone marrow oedema on MR imaging indicates ARCO stage 3 disease in patients with AVN of the femoral head. Eur Radiol. 2014;24(9):2271-2278.
[9] CHEN L, WU Y, CHEN Z, et al. What happens to the gluteus medius in young and middle-aged patients with hip dysplasia? Int Orthop. 2022;46(4):761-768.
[10] LIN T, LI K, CHEN W, et al. Relationship between hip joint medial space ratio and collapse of femoral head in non-traumatic osteonecrosis: a retrospective study. J Hip Preserv Surg. 2021;8(4):311-317.
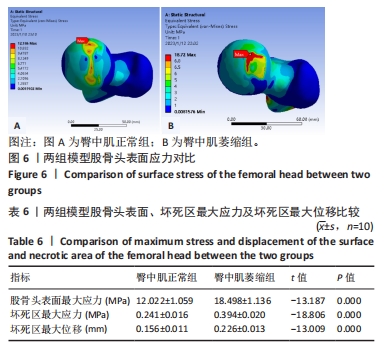
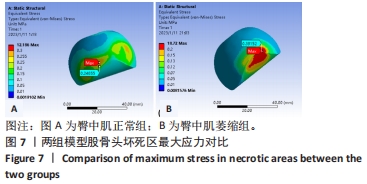
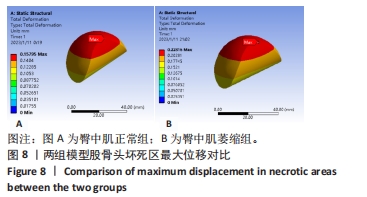
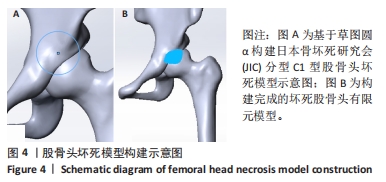
[11] ZHANG Z, LIN T, ZHONG Y, et al. Effect of femoral head necrosis cystic area on femoral head collapse and stress distribution in femoral head: A clinical and finite element study. Open Med (Wars). 2022;17(1):1282-1291.
[12] SVERDLOVA NS, WITZEL U. Principles of determination and verification of muscle forces in the human musculoskeletal system: Muscle forces to minimise bending stress. J Biomech. 2010;43(3):387-396.
[13] GENDA E, KONISHI N, HASEGAWA Y, et al. A computer simulation study of normal and abnormal hip joint contact pressure. Arch Orthop Trauma Surg. 1995;114(4): 202-206.
[14] WINGSTRAND H, WINGSTRAND A. Biomechanics of the hip joint capsule -- a mathematical model and clinical implications. Clin Biomech (Bristol, Avon). 1997;12(5):273-280.
[15] IKEMURA S, MOTOMURA G, KAWANO K, et al. The Discrepancy in the Posterior Boundary of Necrotic Lesion Between Axial and Oblique Axial Slices of MRI in Patients with Osteonecrosis of the Femoral Head. J Bone Joint Surg Am. 2022;104(Suppl 2):33-39.
[16] TAKETA M, FUJII T, KUBOTA H, et al. Correlation between center-edge angle and acetabulum-head index in developmental dysplasia of the hip with avascular necrosis of the femoral head. J Pediatr Orthop B. 2003;12(3):215-218.
[17] TSUTSUMI M, NIMURA A, AKITA K. Clinical anatomy of the musculoskeletal system in the hip region. Anat Sci Int. 2022;97(2):157-164.
[18] 修新军,刘吉华,孙德宝.早期成人股骨头坏死周围软组织病变DR、CT、MRI对比研究[J]. 中华临床医师杂志(电子版),2012,6(6):1556-1558.
[19] HOMMA D, MINATO I, IMAI N, et al. Appropriate sites for the measurement of the cross-sectional area of the gluteus maximus and the gluteus medius muscles in patients with hip osteoarthritis. Surg Radiol Anat. 2021;43(1):45-52.
[20] BAI H, FU YQ, AYENI OR, et al. The anterior hip capsule is thinner in dysplastic hips: a study comparing different young adult hip patients. Knee Surg Sports Traumatol Arthrosc. 2023;31(1):70-78.
[21] SAKI F, TAHAYORI B, BAKHTIARI KS. Female athletes with ligament dominance exhibiting altered hip and ankle muscle co-contraction patterns compared to healthy individuals during single-leg landing. Gait Posture. 2022; 93:225-229.
[22] ABD-ELTAWAB AE, AMEER MA, ELADL MA, et al. Sexual Dimorphism Impact on the Ground Reaction Force Acting on the Mediolateral Direction During Level Walking: Hip Abductor Muscle Biomechanics and Its Correlation to GRF Moment Arm. Front Bioeng Biotechnol. 2022;10:863194.
[23] ZHANG XL, SHEN H, QIN XL, et al. Anterolateral muscle sparing approach total hip arthroplasty: an anatomic and clinical study. Chin Med J (Engl). 2008;121(15):1358-1363.
[24] DAFKOU K, KELLIS E, ELLINOUDIS A, et al. The Effect of Additional External Resistance on Inter-Set Changes in Abdominal Muscle Thickness during Bridging Exercise. J Sports Sci Med. 2020;19(1):102-111.
[25] WIDRICK JJ, FUCHS R, MADDALOZZO GF, et al. Relative effects of exercise training and alendronate treatment on skeletal muscle function of ovariectomized rats. Menopause. 2007;14(3 Pt 1):528-534.
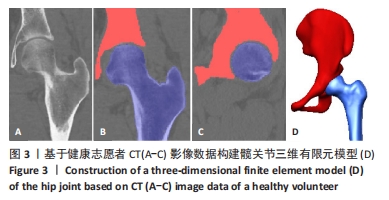
[26] 杨鹏,魏秋实,陈达,等. 基于头臼接触理论构建具有精确软骨受力面的股骨近端三维模型[J]. 广东医学,2017,38(20):3127-3131.
[27] 麻恒源. 唇裂唇鼻肌肉系统三维解剖学研究与唇裂功能性修复的有限元生物力学模似[D]. 北京:北京协和医学院,2016.
[28] WIDRICK JJ, FUCHS R, MADDALOZZO GF, et al. Relative effects of exercise training and alendronate treatment on skeletal muscle function of ovariectomized rats. Menopause. 2007;14(3 Pt 1):528-534.
[29] 陈海诚,陈腾宇,陈国铭,等. 腰腹与髋周肌群差异训练对股骨头坏死保髋的影响[J]. 中华关节外科杂志(电子版),2021,15(3):267-276. |