[1] KIM J, MOON B, KIM D, et al. Postoperative flat back: contribution of posterior accessed lumbar interbody fusion and spinopelvic parameters. J Korean Neurosurg Soc. 2014;56(4):315-322.
[2] DIEBO BG, VARGHESE JJ, LAFAGE R, et al. Sagittal alignment of the spine: what do you need to know? Clin Neurol Neurosurg. 2015;139:295-301.
[3] LEGAYE J, DUVAL-BEAUPÈRE G, HECQUET J, et al. Pelvic incidence: a fundamental pelvic parameter for three‐dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99-103.
[4] FRANK S, PATEL A, UNGAR B, et al. Adult spinal deformity‐postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010; 35:2224-2231.
[5] LIM J, KIM S. Difference of sagittal spinopelvic alignments between degenerative spondylolisthesis and isthmic spondylolisthesis. J Korean Neurosurg Soc. 2013; 53(2):96-101.
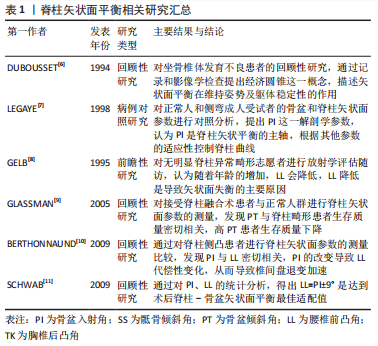
[6] DUBOUSSET J, HADDAD F, ZELLER R, et al. Ischio-vertebral dysplasia (a dangerous syndrome for the spinal cord). Rev Chir Orthop Reparatrice Appar Mot. 1994; 80(7):610-619.
[7] LEGAYE J, DUVAL-BEAUPèRE G, HECQUET J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7(2):99-103.
[8] GELB D, LENKE L, BRIDWELL K, et al. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine (Phila Pa 1976). 1995; 20(12):1351-1358.
[9] GLASSMAN S, BERVEN S, BRIDWELL K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976). 2005; 30(6):682-688.
[10] BERTHONNAUD E, DIMNET J, HILMI R. Classification of pelvic and spinal postural patterns in upright position. Specific cases of scoliotic patients. Comput Med Imaging Graph. 2009;33(8):634-643.
[11] SCHWAB F, LAFAGE V, PATEL A, et al. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976). 2009;34(17):1828-1833.
[12] FENG Y, CHEN L, GU Y, et al. Restoration of the spinopelvic sagittal balance in isthmic spondylolisthesis: posterior lumbar interbody fusion may be better than posterolateral fusion. Spine J. 2015;15(7):1527-1535.
[13] LE HUEC J, THOMPSON W, MOHSINALY Y, et al. Sagittal balance of the spine. Eur Spine J. 2019;28(9):1889-1905.
[14] LENG Y, TANG C, LIAO Y, et al. Correlation between sacral slope and pedicle morphology of the fourth lumbar vertebra in degenerative lumbar spondylolisthesis. Global Spine J. 2022. doi: 10.1177/21925682221117151.
[15] BERVEN S, WADHWA R. Sagittal alignment of the lumbar spine. Neurosurg Clin N Am. 2018;29(3):331-339.
[16] CHOI S, SON S, LEE D, et al. L1 incidence reflects pelvic incidence and lumbar lordosis mismatch in sagittal balance evaluation. Medicine (Baltimore). 2018; 97(30):e11668.
[17] BOULAY C, TARDIEU C, HECQUET J, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15(4):415-422.
[18] SENTELER M, WEISSE B, SNEDEKER J, et al. Pelvic incidence-lumbar lordosis mismatch results in increased segmental joint loads in the unfused and fused lumbar spine. Eur Spine J. 2014;23(7):1384-1393.
[19] TANG C, LIAO Y, TANG Q, et al. What is the difference in pedicle morphology of the fifth lumbar vertebra between isthmic and degenerative L5-S1 spondylolisthesis? An anatomic study of 328 patients via multi-slice spiral computed tomography. Eur Spine J. 2021;30(8):2301-2310.
[20] RADOVANOVIC I, URQUHART J, GANAPATHY V, et al. Influence of postoperative sagittal balance and spinopelvic parameters on the outcome of patients surgically treated for degenerative lumbar spondylolisthesis. J Neurosurg Spine. 2017;26(4):448-453.
[21] KOBAYASHI H, ENDO K, SAWAJI Y, et al. Global sagittal spinal alignment in patients with degenerative low-grade lumbar spondylolisthesis. J Orthop Surg (Hong Kong). 2019;27(3):2309499019885190.
[22] OIKONOMIDIS S, MEYER C, SCHEYERER M, et al. Lumbar spinal fusion of low-grade degenerative spondylolisthesis (Meyerding grade I and II): do reduction and correction of the radiological sagittal parameters correlate with better clinical outcome? Arch Orthop Trauma Surg. 2020;140(9):1155-1162.
[23] BERNARD F, MAZERAND E, GALLET C, et al. History of degenerative spondylolisthesis: from anatomical description to surgical management. Neurochirurgie. 2019;65:75-82.
[24] KEPLER C, VACCARO A, HILIBRAND A, et al. National trends in the use of fusion techniques to treat degenerative spondylolisthesis. Spine (Phila Pa 1976). 2014; 39(19):1584-1589.
[25] LAN T, HU S, ZHANG Y, et al. Comparison between posterior lumbar interbody fusion and transforaminal lumbar interbody fusion for the treatment of lumbar degenerative diseases: a systematic review and meta-analysis. World Neurosurg. 2018;112:86-93.
[26] YE Y, XU H, CHEN D. Comparison between posterior lumbar interbody fusion and posterolateral fusion with transpedicular screw fixation for isthmic spondylolithesis:a meta-analysis. Arch Orthop Trauma Surg. 2013;133(12):1649-1655.
[27] FALDINI C, BARILE F, IALUNA M, et al. High-grade dysplastic spondylolisthesis: surgical technique and case series. Musculoskelet Surg. 2022. doi: 10.1007/s12306-022-00763-w.
[28] PHAN K, NAZARETH A, HUSSAIN A, et al. Relationship between sagittal balance and adjacent segment disease in surgical treatment of degenerative lumbar spine disease:meta-analysis and implications for choice of fusion technique. Eur Spine J. 2018;27(8):1981-1991.
[29] LEE J, KIM Y, SOH J, et al. Risk factors of adjacent segment disease requiring surgery after lumbar spinal fusion:comparison of posterior lumbar interbody fusion and posterolateral fusion. Spine (Phila Pa 1976). 2014;39(5):E339-E345.
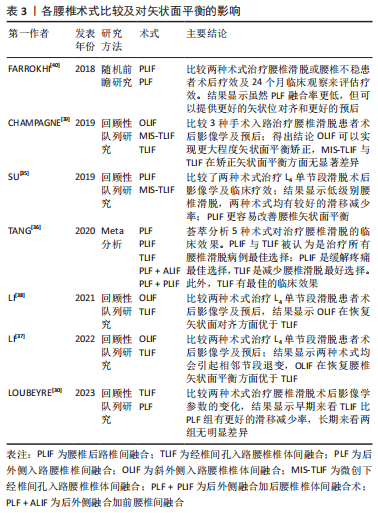
[30] LOUBEYRE J, FERRERO E, JMAL M, et al. Surgical treatment of degenerative lumbar spondylolisthesis: effect of TLIF and slip reduction on sagittal alignment. Orthop Traumatol Surg Res. 2023. doi: 10.1016/j.otsr.2022.103541.
[31] GLASSMAN S, BRIDWELL K, DIMAR J, et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30(18):2024-2029.
[32] ELMORSY S, ABULNASR H, HASSAN Y, et al. Functional outcome of surgical management of low mid-grade lumbar spondylolisthesis when considering the sagittal balance parameters preoperatively:a prospective study. Chin Neurosurg J. 2022;8(1):35.
[33] LEVEQUE J, DROLET C, NEMANI V, et al. The impact of surgical approach on sagittal plane alignment in patients undergoing one- or two- level fusions for degenerative pathology: a multicenter radiographic evaluation 6 months following surgery. World Neurosurg. 2022;164:e311-e317.
[34] O’CONNOR B, DROLET C, LEVEQUE J, et al. The impact of interbody approach and lumbar level on segmental, adjacent, and sagittal alignment in degenerative lumbar pathology:a radiographic analysis six months following surgery. Spine J. 2022;22(8):1318-1324.
[35] SU K, LUAN J, WANG Q, et al. Radiographic analysis of minimally invasive transforaminal lumbar interbody fusion versus conventional open surgery on sagittal lumbar-pelvic alignment for degenerative spondylolisthesis. World Neurosurg. 2019;124:e733-e739.
[36] TANG L, WU Y, JING D, et al. A Bayesian network meta-analysis of 5 different fusion surgical procedures for the treatment of lumbar spondylolisthesis. Medicine (Baltimore). 2020;99(14):e19639.
[37] LI G, TONG T, WANG L. Comparative analysis of the effects of OLIF and TLIF on adjacent segments after treatment of L4 degenerative lumbar spondylolisthesis. J Orthop Surg Res. 2022;17(1):203.
[38] LI R, SHAO X, LI X, et al. Comparison of clinical outcomes and spino-pelvic sagittal balance in degenerative lumbar spondylolisthesis: minimally invasive oblique lumbar interbody fusion (OLIF) versus transforaminal lumbar interbody fusion (TLIF). Medicine (Baltimore). 2021;100(3):e23783.
[39] CHAMPAGNE P, WALSH C, DIABIRA J, et al. Sagittal balance correction following lumbar interbody fusion: a comparison of the three approaches. Asian Spine J. 2019;13(3):450-458.
[40] FARROKHI M, YADOLLAHIKHALES G, GHOLAMI M, et al. Clinical outcomes of posterolateral fusion vs. posterior lumbar interbody fusion in patients with lumbar spinal stenosis and degenerative instability. Pain physician. 2018;21(4):383-406.
[41] LI Y, WU Z, GUO D, et al. A comprehensive comparison of posterior lumbar interbody fusion versus posterolateral fusion for the treatment of isthmic and degenerative spondylolisthesis: a meta-analysis of prospective studies. Clin Neurol Neurosurg. 2020;188:105594.
[42] UEHARA M, TAKAHASHI J, IKEGAMI S, et al. Determination of optimal screw number based on correction angle for main thoracic curve in adolescent idiopathic scoliosis. J J Orthop Sci. 2019;24(3):415-419.
[43] MATSUKAWA K, YATO Y, IMABAYASHI H. Impact of screw diameter and length on pedicle screw fixation strength in osteoporotic vertebrae: a finite element analysis. Asian Spine J. 2021;15(5):566-574.
[44] ZHOU Q, ZHANG J, ZHENG Y, et al. Effects of different pedicle screw insertion depths on sagittal balance of lumbar degenerative spondylolisthesis, a retrospective comparative study. BMC Musculoskelet Disord. 2021;22(1):850.
[45] KARIM S, FISHER C, GLENNIE A, et al. Preoperative patient-reported outcomes are not associated with sagittal and spinopelvic alignment in degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976). 2022;47(16):1128-1136.
[46] MELIKIAN R, YOON S, KIM J, et al. Sagittal plane correction using the lateral transpsoas approach: a biomechanical study on the effect of cage angle and surgical technique on segmental lordosis. Spine (Phila Pa 1976). 2016;41(17): E1016-E1021.
[47] ALAHMARI A, THORNLEY P, GLENNIE A, et al. Preoperative disc angle is an important predictor of segmental lordosis after degenerative spondylolisthesis fusion. Global Spine J. 2022. doi: 10.1177/21925682221118845.
[48] KAITO T, HOSONO N, FUJI T, et al. Disc space distraction is a potent risk factor for adjacent disc disease after PLIF. Arch Orthop Trauma Surg. 2011;131(11):1499-1507.
[49] CHEH G, BRIDWELL K, LENKE L, et al. Adjacent segment disease followinglumbar/thoracolumbar fusion with pedicle screw instrumentation:a minimum 5-year follow-up. Spine (Phila Pa 1976). 2007;32(20):2253-2257.
[50] SCHULTE T, LEISTRA F, BULLMANN V, et al. Disc height reduction in adjacent segments and clinical outcome 10 years after lumbar 360 degrees fusion. Eur Spine J. 2007;16(12):2152-2158.
[51] KUMAR M, JACQUOT F, HALL H. Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J. 2001;10(4):309-313.
[52] SHAO X, LIU H, WU J, et al. A retrospective comparative study of postoperative sagittal balance in isthmic L5-S1 spondylolisthesis using single segment or two-segment pedicle screw fixation. BMC Musculoskelet Disord. 2022;23(1):145.
[53] SEARS W, SERGIDES I, KAZEMI N, et al. Incidence and prevalence of surgery at segments adjacent to a previous posterior lumbar arthrodesis. Spine J. 2011; 11(1):11-20.
[54] BAE JS, LEE SH, KIM JS, et al. Adjacent segment degeneration after lumbar interbody fusion with percutaneous pedicle screw fixation for adult low-grade isthmic spondylolisthesis: minimum 3 years of follow-up. Neurosurgery. 2010; 67(6):1600-1608.
[55] WEGMANN K, GUNDERMANN S, SIEWE J, et al. Correlation of reduction and clinical outcome in patients with degenerative spondylolisthesis. Arch Orthop Trauma Surg. 2013;133(12):1639-1644.
[56] SOH J, LEE J, SHIN B. Analysis of risk factors for adjacent segment degeneration occurring more than 5 years after fusion with pedicle screw fixation for degenerative lumbar spine. Asian Spine J. 2013;7(4):273-281.
[57] KAWAKAMI M, TAMAKI T, ANDO M, et al. Lumbar sagittal balance influences the clinical outcome after decompression and posterolateral spinal fusion for degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976). 2002;27(1):59-64.
[58] JASINSKI J, TONG D, HANSON C, et al. Sagittal adjusting screws for the correction of grade IV spondylolisthesis in a patient with Ehlers-Danlos syndrome:illustrative case. J Neurosurg Case Lessons. 2021;2(2):CASE21196.
[59] LAMBRECHTS M, BARBER J, BECKETT N, et al. Surgical reduction of spondylolisthesis during lumbar fusion:are complications associated with slip correction? Clin Spine Surg. 2022;35(1):E1-E6.
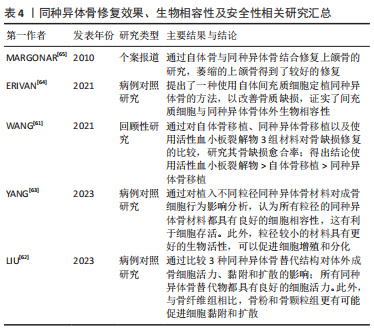
[60] CAKIR T, YOLAS C. Synthetic bone graft versus autograft obtained from the spinous process in posterior lumbar interbody fusion. Turk Neurosurg. 2021;31(2):199-205.
[61] WANG Q, HUANG Z, HUANG X, et al. Reparative effect of super active platelet combined with allogeneic bone for large bone defects. Artif Organs. 2021;45(10): 1219-1228.
[62] LIU J, YANG L, ZHANG H, et al. Effects of allogeneic bone substitute configurations on cell adhesion process in vitro. J Orthop Surg. 2023;15(2):579-590.
[63] YANG L, ZHANG H, LIU J, et al. Relative influence on cell behaviors of osteoblasts seeded onto demineralized bone matrix with diverse particle size. Cell and tissue banking. 2023; 24(2): 369-385.
[64] ERIVAN R, SAMPER N, VILLATTE G, et al. No detectable alteration of inorganic allogeneic bone matrix colonizing mesenchymal cells: a step towards personalized bone grafts. J Bone Metab. 2021;28(2):161-169.
[65] MARGONAR R, DOS SANTOS P, QUEIROZ T, et al. Rehabilitation of atrophic maxilla using the combination of autogenous and allogeneic bone grafts followed by protocol-type prosthesis. J Craniofac Surg. 2010;21(6):1894-1896.
[66] MATSUMOTO K, SHAH A, KELKAR A, et al. Sagittal imbalance may lead to higher risks of vertebral compression fractures and disc degeneration-a finite element analysis. World Neurosurg. 2022;167:e962-e971.
[67] LAFAGE V, SCHWAB F, VIRA S, et al. Spino-pelvic parameters after surgery can be predicted: a preliminary formula and validation of standing alignment. Spine (Phila Pa 1976). 2011;36(13):1037-1045. |