中国组织工程研究 ›› 2021, Vol. 25 ›› Issue (36): 5821-5826.doi: 10.12307/2021.349
• 脊柱植入物 spinal implant • 上一篇 下一篇
椎间自体骨植骨面积比与椎间融合率的关系
唐 强,钟德君,王 清,廖晔晖,唐 超,马 飞
- 西南医科大学附属医院骨科,四川省泸州市 646000
Relationship between area ratio of interbody autograft and intervertebral fusion rate
Tang Qiang, Zhong Dejun, Wang Qing, Liao Yehui, Tang Chao, Ma Fei
- Department of Orthopedics, Affiliated Hospital of Southwest Medical University, Luzhou 646000, Sichuan Province, China
摘要:
文题释义:
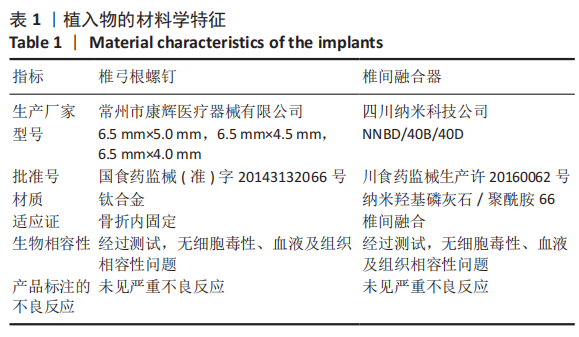
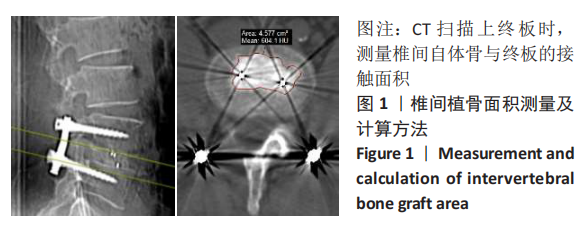
椎间自体骨植骨面积比:融合节段椎间自体骨植骨与上、下终板接触的横截面积与之相应接触终板面积的比值×100%,取其均值。背景:目前相关报道认为椎间植骨体积是影响椎间融合率的因素之一,但相同植骨体积因个体差异导致椎间植骨与终板的接触面积不同,椎间植骨与终板的接触面积对椎间融合率的影响鲜有分析研究。
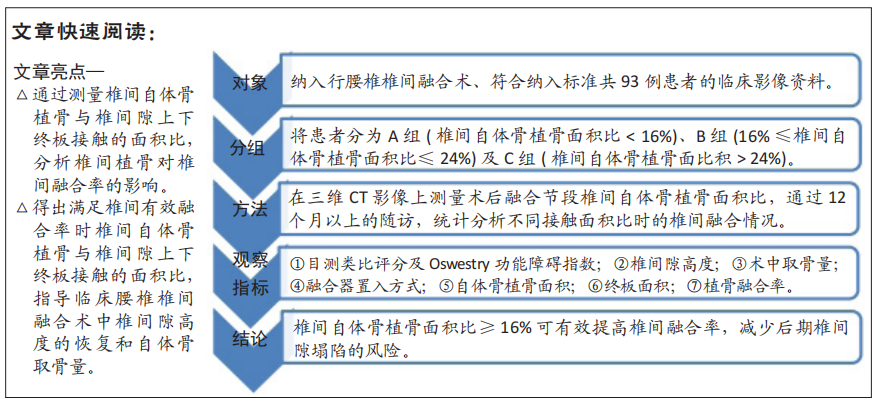
目的:探讨行腰椎后路椎间融合时自体骨植骨面积比对椎间融合率的影响。
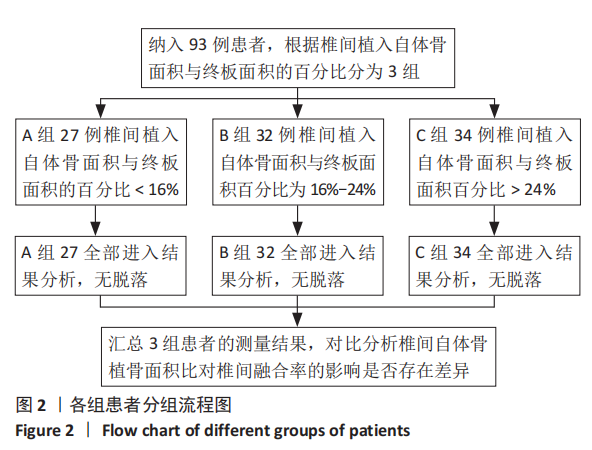
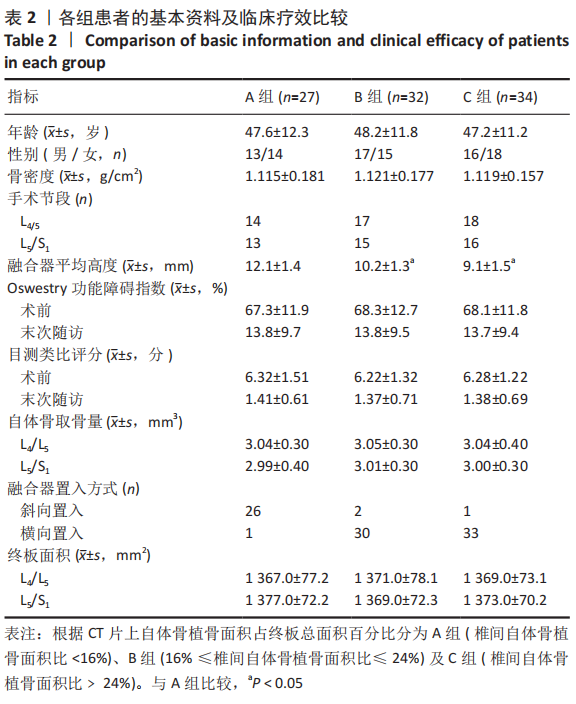
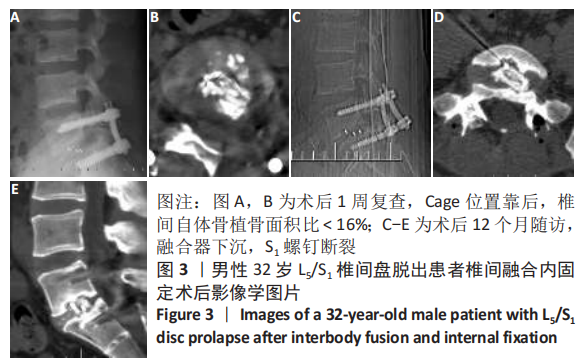
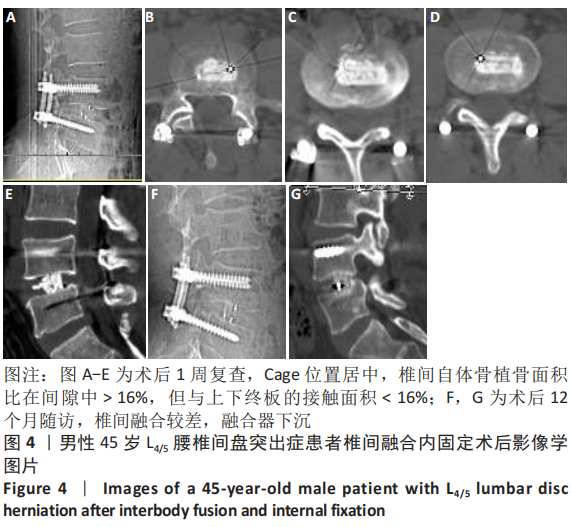
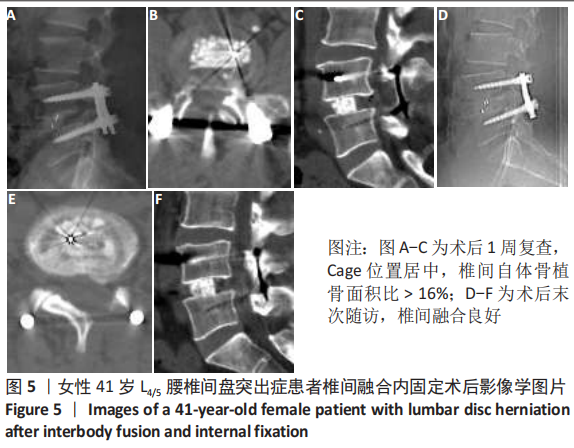
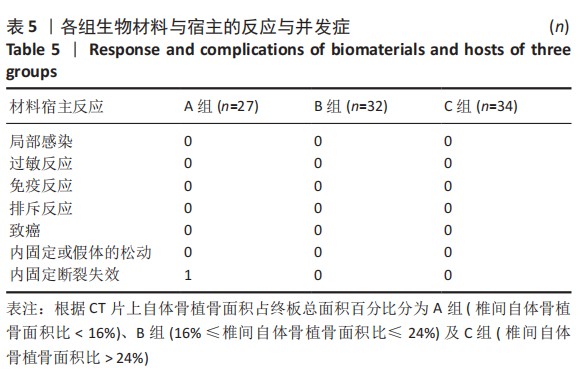
方法:回顾性分析2017年1月至2018年12月在西南医科大学附属医院脊柱外科行腰椎后路椎体间融合手术且符合纳入标准共93例患者的临床资料,记录患者术前椎间隙高度、上下终板面积、Oswestry功能障碍指数及目测类比评分、术中使用Cage大小及自体骨取骨量,术后测量自体骨植骨面积(椎间与上下终板接触的自体骨面积),取其均值;根据术后1周测量的自体骨植骨面积占终板总面积百分比分为A组(椎间自体骨植骨面积比< 16%)、B组(16%≤椎间自体骨植骨面积比≤24%)及C组(椎间自体骨植骨面积比> 24%)。术后6,12 个月及末次随访行X射线片及CT检查,观察3组患者术中融合器置入方向,记录随访时椎间隙高度、椎间自体骨植骨面积比、椎间融合Brantigan评分、Oswestry功能障碍指数及目测类比评分。测量由2名脊柱外科医师分别完成,间隔1周重复测量,检验观察者间及观察者内信度。比较分析椎间自体骨植骨面积对椎间融合率的影响。
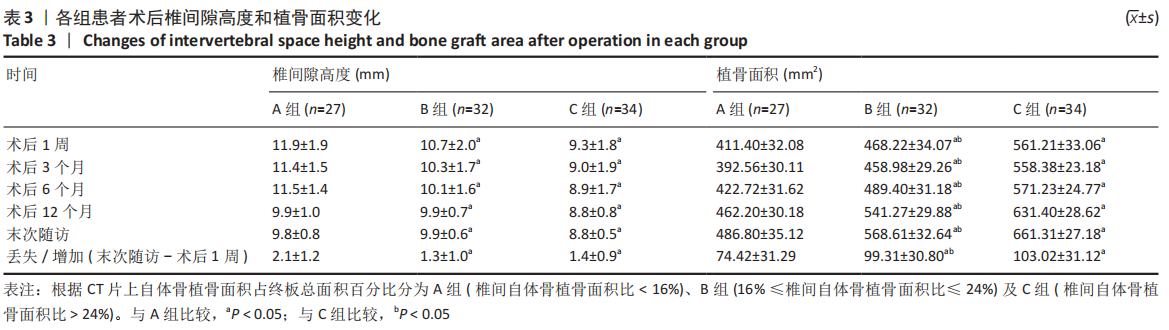
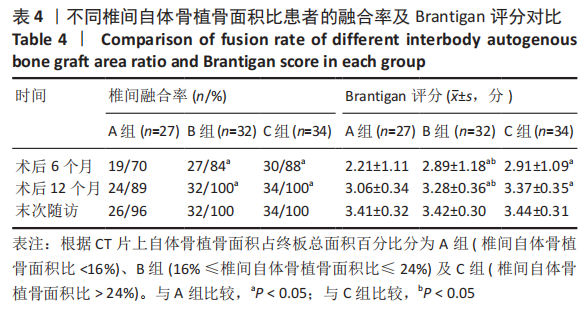
结果与结论:①椎间植骨面积测量结果观察者间及观察者内信度分别为0.924和0.913;②所有患者均获得12个月以上随访,3组患者年龄、性别及手术节段差异均无显著性意义(P > 0.05),术前椎间隙高度、Oswestry功能障碍指数及目测类比评分组间比较差异无显著性意义(P > 0.05);③A组患者27例,其中融合器斜向置入26例,横向置入1例;B组患者32例,其中融合器斜向置入2例,横向置入30例;C组患者34例,斜向置入1例,横向置入33例;④3组患者术中自体骨取骨量比较差异无显著性意义(P > 0.05);术后1周椎间隙平均高度A组大于B、C组(P=0.022,P=0.000),自体骨植骨面积A组小于B、C组(P=0.000,P=0.000);⑤术后6个月及12个月,椎间融合率A组(70.4%,88.9%)低于B组(84.4%,100%)和C组(88.2%,100%),Brantigan评分A组低于B组(P=0.027,P=0.020)和C组(P=0.018,P=0.001);⑥末次随访3组患者Oswestry功能障碍指数及目测类比评分比较差异均无显著性意义(P > 0.314),椎间隙高度丢失A组大于B、C组(P=0.007,P=0.013),椎间植骨融合成骨增加面积A组低于B、C组(P=0.003,P=0.000),3组融合率及Brantigan评分比较差异无显著性意义(P=0.902,P=0.712);⑦提示椎间自体骨植骨面积比≥16%可有效提高椎间融合率,减少后期椎间隙塌陷的风险。
https://orcid.org/0000-0002-3776-9695 (唐强)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号: