| [1] Sánchez-Miralles A, Castellanos G, Badenes R, et al. Abdominal compartment syndrome and acute intestinal distress syndrome.Med Intensiva. 2013;37(2):99-109.
[2] Guzel A, Kanter M, Guzel A, et al. Protective effect of curcumin on acute lung injury induced by intestinal ischaemia/reperfusion.Toxicol Ind Health. 2013;29(7): 633-642.
[3] Baker B, Maitra U, Geng S, et al. Molecular and cellular mechanisms responsible for cellular stress and low-grade inflammation induced by a super-low dose of endotoxin. J Biol Chem. 2014;289(23): 16262-16269.
[4] Ariga SK, Abatepaulo FB, Melo ES, et al. Endotoxin tolerance drives neutrophil to infectious site. Shock. 2014;42(2):168-173.
[5] Andersson U, Tracey KJ. HMGB1 is a therapeutic target for sterile inflammation and infection. Annu Rev Immunol. 2011;29:139-162.
[6] He GZ, Zhou KG, Zhang R, et al. The effects of n-3 PUFA and intestinal lymph drainage on high-mobility group box 1 and Toll-like receptor 4 mRNA in rats with intestinal ischaemia-reperfusion injury. Br J Nutr. 2012; 108(5):883-892.
[7] Ben DF, Yu XY, Ji GY, et al. TLR4 mediates lung injury and inflammation in intestinal ischemia-reperfusion. J Surg Res. 2012;174(2):326-333.
[8] Wohlauer MV, Moore EE, Harr J, et al. Cross-transfusion of postshock mesenteric lymph provokes acute lung injury. J Surg Res. 2011;170(2): 314-318.
[9] Kim SI, Kim YB, Koh KM, et al. Activation of NF-κB pathway in oral buccal mucosa during small intestinal ischemia-reperfusion injury. J Surg Res. 2013;179(1): 99-105.
[10] Deitch EA. Gut lymph and lymphatics: a source of factors leading to organ injury and dysfunction. Ann N Y Acad Sci. 2010;1207 Suppl 1:E103-111.
[11] He GZ, Zhou KG, Zhang R, et al. Impact of intestinal ischemia/reperfusion and lymph drainage on distant organs in rats. World J Gastroenterol. 2012;18(48): 7271-7278.
[12] He GZ, Dong LG, Chen XF, et al. Lymph duct ligation during ischemia/reperfusion prevents pulmonary dysfunction in a rat model with ω-3 polyunsaturated fatty acid and glutamine. Nutrition. 2011;27(5): 604-614.
[13] Yoshiya K, Lapchak PH, Thai TH, et al. Depletion of gut commensal bacteria attenuates intestinal ischemia/ reperfusion injury.Am J Physiol Gastrointest Liver Physiol. 2011;301(6):G1020-1030.
[14] Zhang WX, Zhou LF, Zhang L, et al. Protective effects of glutamine preconditioning on ischemia-reperfusion injury in rats. Hepatobiliary Pancreat Dis Int. 2011;10(1):78-82.
[15] Krauss H, Bogdański P, Sosnowski P, et al. Influence of short-term L-arginine supplementation on carbohydrate balance in rats with ischemia-reperfusion syndrome. Pharmacol Rep. 2012;64(3):635-642.
[16] Schaffer SW, Jong CJ, Ito T, et al. Effect of taurine on ischemia-reperfusion injury. Amino Acids. 2014;46(1): 21-30.
[17] Friedenstein AJ, Gorskaja JF, Kulagina NN. Fibroblast precursors in normal and irradiated mouse hematopoietic organs. Exp Hematol. 1976;4(5):267-274.
[18] Woodbury D, Reynolds K, Black IB. Adult bone marrow stromal stem cells express germline, ectodermal, endodermal, and mesodermal genes prior to neurogenesis. J Neurosci Res. 2002;69(6):908-917.
[19] Jiang Y, Jahagirdar BN, Reinhardt RL, et al. Pluripotency of mesenchymal stem cells derived from adult marrow. Nature. 2002;418(6893):41-49.
[20] Mouiseddine M, François S, Semont A, et al. Human mesenchymal stem cells home specifically to radiation-injured tissues in a non-obese diabetes/ severe combined immunodeficiency mouse model. Br J Radiol. 2007;80 Spec No 1:S49-55.
[21] Chapel A, Bertho JM, Bensidhoum M, et al. Mesenchymal stem cells home to injured tissues when co-infused with hematopoietic cells to treat a radiation-induced multi-organ failure syndrome. J Gene Med. 2003;5(12):1028-1038.
[22] Shi M, Li J, Liao L, et al. Regulation of CXCR4 expression in human mesenchymal stem cells by cytokine treatment: role in homing efficiency in NOD/SCID mice. Haematologica. 2007;92(7):897-904.
[23] Dar A, Kollet O, Lapidot T. Mutual, reciprocal SDF-1/CXCR4 interactions between hematopoietic and bone marrow stromal cells regulate human stem cell migration and development in NOD/SCID chimeric mice. Exp Hematol. 2006;34(8):967-975.
[24] De Miguel MP, Fuentes-Julián S, Blázquez-Martínez A, et al. Immunosuppressive properties of mesenchymal stem cells: advances and applications. Curr Mol Med. 2012;12(5):574-591.
[25] Liu J, Guo Y, Mu Y, et al.Infusion of mesenchymal stem cells ameliorates hyperglycemia in type 2 diabetic rats: identification of a novel role in improving insulin sensitivity. Diabetes. 2012;61(6):1616-1625.
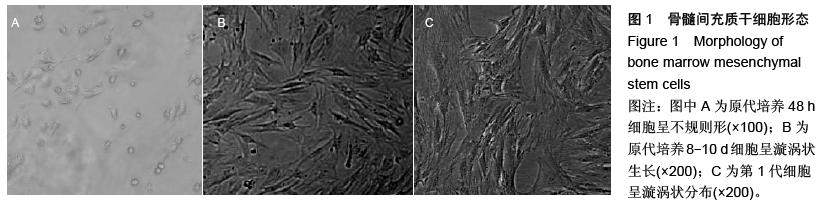
[26] 李晓峰,赵劲民,苏伟,等.大鼠骨髓间充质干细胞的培养与鉴定[J].中国组织工程研究与临床康复,2011,15(10): 1721-1725.
[27] 范萍,刘永琦,吴晓晶,等.不同条件下骨髓间充质干细胞分离培养及其生物学特性研究[J].细胞与分子免疫学杂志, 2010,26(4):322-324.
[28] 谢杏榕,李云静,李儒贵,等.胚胎肝细胞提取液体外诱导骨髓干细胞向肝系细胞分化的实验研究[J].现代预防医学, 2013,40(1):124-126.
[29] 齐丙迪,孟宝玺,杨阳,等.第三方骨髓间充质干细胞诱导同种异体移植受体免疫耐受机制的研究[J].中华整形外科杂志,2011,27(3):207-212.
[30] 续玉林,李刚,吕小东,等.骨髓间充质干细胞移植调节TNF-α和IL-10浓度减轻八稀酸诱导的大鼠急性肺损伤[J].心肺血管病杂志,2012,31(3):324-327.
[31] 周锐,周元平,郑玲,等.骨髓间充质干细胞移植对大鼠爆发性肝功能衰竭治疗作用的初步观察[J].中华传染病杂志, 2012,30(2):85-89.
[32] 董晨,杨焕丹,丰炳峰,等.骨髓间充质干细胞对阿霉素肾病大鼠肾脏nephrin表达的影响[J].中国组织工程研究与临床康复,2010,14(32):5897-5902.
[33] Nezhadi A, Ghazi F, Rassoli H, et al. BMSC and CoQ10 improve behavioural recovery and histological outcome in rat model of Parkinson's disease. Pathophysiology. 2011;18(4):317-324.
[34] 陈丹丹,付文玉,庄宝祥,等.骨髓间充质干细胞黑质内移植对帕金森病大鼠的治疗作用[J].中国实验动物学报,2013, 21(1):22-26.
[35] 赵学俊.自体骨髓间充质干细胞移植在中枢神经系统疾病中的应用[J].中国实用神经疾病杂志,2012,15(8): 69-70.
[36] Miller RH, Bai L, Lennon DP, et al. The potential of mesenchymal stem cells for neural repair. Discov Med. 2010;9(46):236-242.
[37] 符星,石贞玉,金海啸,等.海马微环境对细胞分化和极性化的影响[J].解剖学报,2013,44(5):586-593.
[38] Li YP, Paczesny S, Lauret E, et al. Human mesenchymal stem cells license adult CD34+ hemopoietic progenitor cells to differentiate into regulatory dendritic cells through activation of the Notch pathway. J Immunol. 2008;180(3):1598-1608.
[39] Jeschke MG, Bolder U, Finnerty CC, et al. The effect of hepatocyte growth factor on gut mucosal apoptosis and proliferation, and cellular mediators after severe trauma. Surgery. 2005;138(3):482-489.
[40] Hayashi Y, Tsuji S, Tsujii M, et al. Topical transplantation of mesenchymal stem cells accelerates gastric ulcer healing in rats. Am J Physiol Gastrointest Liver Physiol. 2008;294(3):G778-786.
[41] Song H, Kwon K, Lim S, et al. Transfection of mesenchymal stem cells with the FGF-2 gene improves their survival under hypoxic conditions. Mol Cells. 2005;19(3):402-407.
[42] Weil BR, Markel TA, Herrmann JL, et al. Mesenchymal stem cells enhance the viability and proliferation of human fetal intestinal epithelial cells following hypoxic injury via paracrine mechanisms. Surgery. 2009;146(2): 190-197. |
.jpg)
.jpg)
.jpg)
.jpg)