[1] CENTERS FOR DISEASE CONTROL AND PREVENTION (CDC). Prevalence and most common causes of disability among adults--United States, 2005. MMWR Morb Mortal Wkly Rep. 2009;58(16):421-426.
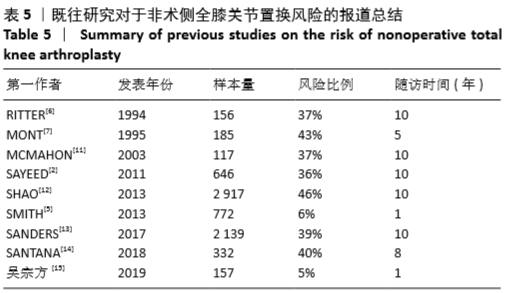
[2] SAYEED SA, SAYEED YA, BARNES SA, et al. The risk of subsequent joint arthroplasty after primary unilateral total knee arthroplasty, a 10-year study. J Arthroplasty. 2011;26(6):842-846.
[3] PARISI TJ, LEVY DL, DENNIS DA, et al. Radiographic changes in nonoperative contralateral knee after unilateral total knee arthroplasty. J Arthroplasty. 2018; 33(7S): S116-S120.
[4] 时超, 李朝顶, 罗仲伟, 等. 分期和同期全膝关节置换手术的临床效果观察[J]. 实用骨科杂志, 2016,22(12): 1069-1072,1076.
[5] SMITH HK, WYLDE V, LINGARD EA, et al. The effect of pain after total knee arthroplasty on the contralateral, nonreplaced knee. J Bone Joint Surg Am. 2013;95(4):315-322.
[6] RITTER MA, CARR KD, KEATING EM, et al. Long-term outcomes of contralateral knees after unilateral total knee arthroplasty for osteoarthritis. J Arthroplasty. 1994;9(4):347-349.
[7] MONT MA, MITZNER DL, JONES LC, et al. History of the contralateral knee after primary knee arthroplasty for osteoarthritis. Clin Orthop Relat Res. 1995;(321):145-150.
[8] 唐金龙, 杨冠杰, 刘磊, 等. 全膝关节置换后双下肢长度及相关功能变化[J]. 中国组织工程研究, 2020, 24(15):2310-2316.
[9] ZAHN RK, FUSSI J, VON ROTH P, et al. Postoperative Increased Loading Leads to an Alteration in the Radiological Mechanical Axis After Total Knee Arthroplasty. J Arthroplasty. 2016; 31(8):1803-1807.
[10] HASHIMOTO S, TERAUCHI M, HATAYAMA K, et al. Younger patients with high varus malalignment of the contralateral knee may be candidates for simultaneous bilateral total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019;27(7):2173-2180.
[11] MCMAHON M, BLOCK JA. The risk of contralateral total knee arthroplasty after knee replacement for osteoarthritis. J Rheumatol. 2003;30(8):1822-1824.
[12] SHAO Y, ZHANG C, CHARRON KD, et al. The fate of the remaining knee(s) or hip(s) in osteoarthritic patients undergoing a primary TKA or THA. J Arthroplasty. 2013;28(10):1842-1845.
[13] SANDERS TL, MARADIT KREMERS H, SCHLECK CD, et al. Subsequent total joint arthroplasty after primary total knee or hip arthroplasty: a 40-year population-based study. J Bone Joint Surg Am. 2017; 99(5): 396-401.
[14] SANTANA DC, ANIS HK, MONT MA, et al. What is the Likelihood of Subsequent Arthroplasties after Primary TKA or THA? Data from the Osteoarthritis Initiative. Clin Orthop Relat Res. 2020; 478(1): 34-41.
[15] 吴宗方, 秦江辉, 蒋青, 等.膝关节骨关节炎患者行单侧膝关节置换术后对侧膝关节力线的变化[J]. 实用骨科杂志, 2019, 25(2): 117-122.
[16] WOLFE F, LANE NE. The longterm outcome of osteoarthritis: rates and predictors of joint space narrowing in symptomatic patients with knee osteoarthritis. J Rheumatol. 2002;29(1): 139-146.
[17] FELSON DT, ANDERSON JJ, NAIMARK A, et al. Obesity and knee osteoarthritis. The Framingham Study. Ann Intern Med. 1988;109(1): 18-24.
[18] NIU J, ZHANG YQ, TORNER J, et al. Is obesity a risk factor for progressive radiographic knee osteoarthritis. Arthritis Rheum. 2009;61(3): 329-335.
[19] MAK WK, BIN ABD RAZAK HR, TAN HA. Which patients require a contralateral total knee arthroplasty within 5 years of index surgery. J Knee Surg. 2019.doi: 10.1055/s-0039-1692653.
[20] 李琳, 林坚, 刘晓林, 等. 髋膝踝关节周围肌群肌力训练对老年全膝关节置换术后患者下肢运动功能的影响[J]. 中国康复医学杂志, 2018,33(4):436-440.
[21] FARQUHAR S, SNYDER-MACKLER L. The Chitranjan Ranawat Award: The nonoperated knee predicts function 3 years after unilateral total knee arthroplasty. Clin Orthop Relat Res. 2010;468(1): 7-44.
[22] MAXWELL J, NIU J, SINGH JA, et al. The influence of the contralateral knee prior to knee arthroplasty on post-arthroplasty function: the multicenter osteoarthritis study. J Bone Joint Surg Am. 2013; 95(11): 989-993.
[23] 赵峰, 裴征, 刘亮, 等. 骨关节炎患者单侧膝关节置换对非术侧膝功能变化的影响分析[J]. 河北医药, 2017, 39(12):1880-1883. |
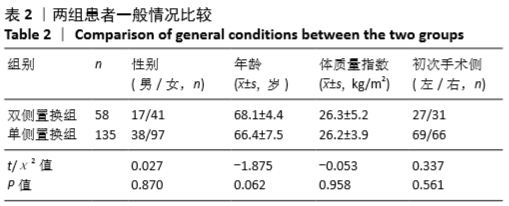
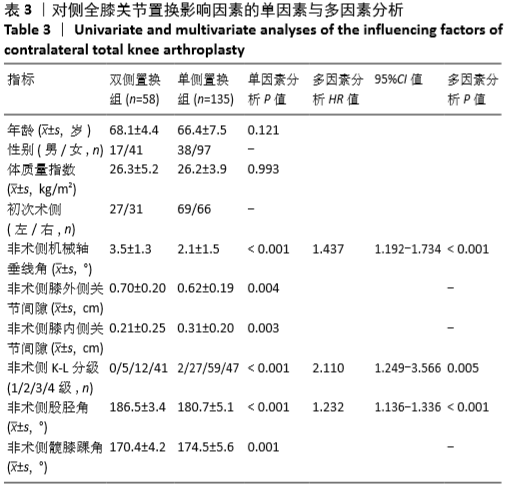

 尽管体质量指数、性别、年龄等与骨性关节炎的发生和进展有关[5],但此次研究发现这些因素与将来对侧膝行全膝关节置换的风险并没有关联。体质量指数高的女性患者确实更容易患骨关节炎[16],体质量指数与骨关节炎的关系在既往文献中已经得到证实,体质量指数的增加会导致膝关节压力增大,进而促使软骨分解、骨赘形成、软骨下骨肥大,并最终导致关节破坏[17-18]。但一旦确诊为双膝骨关节炎以后,这些因素对其未来的进展并没有显著的影响。
尽管体质量指数、性别、年龄等与骨性关节炎的发生和进展有关[5],但此次研究发现这些因素与将来对侧膝行全膝关节置换的风险并没有关联。体质量指数高的女性患者确实更容易患骨关节炎[16],体质量指数与骨关节炎的关系在既往文献中已经得到证实,体质量指数的增加会导致膝关节压力增大,进而促使软骨分解、骨赘形成、软骨下骨肥大,并最终导致关节破坏[17-18]。但一旦确诊为双膝骨关节炎以后,这些因素对其未来的进展并没有显著的影响。