[1] GOEL A , BHATJIWALE M , DESAI K. Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg. 1998;88(6):962-968.
[2] 唐军伟. 颅底凹陷症分型及对手术式选择的意义[D].乌鲁木齐:新疆医科大学,2010.
[3] ATUL G. Atlanto-axial joint distraction in the treatment of select cases of basilar invagination, syringomyelia and fixed atlanto-axial dislocation. Nepal J Neurosci. 2005; 2:1-6.
[4] KLIMO P JR, RAO G, BROCKMEYER D. Congenital anomalies of the cervical spine. Neurosurg Clin N Am. 2007;18(3) :463-478.
[5] SAWIN PD , MENEZES AH. Basilar invagination in osteogenesis imperfecta and related osteochondrodysplasias: medical and surgical management. J Neurosurg. 1997;86(6):950-960.
[6] GOEL A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine. 2004;1(3):281-286.
[7] WANG C , YAN M , ZHOU HT , et al. Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine. 2006;31(11):E306-E313.
[8] DING X , ABUMI K , ITO M , et al. A retrospective study of congenital osseous anomalies at the craniocervical junction treated by occipitocervical plate-rod systems. Eur Spine J. 2012;21(8):1580-1589.
[9] PAN J , HUANG D , HAO D , et al. Occipitocervical fusion: Fix to C2 or C3? Clin Neurol Neurosurg. 2014;127:134-139.
[10] MATSUNAGA S, ONISHI T, SAKOU T. Significance of occipitoaxial angle in subaxial lesion after occipitocervical fusion. Spine. 2001;26(2):161-165.
[11] LOGROSCINO CA, GENITIEMPO M, CASULA S. Relevance of the cranioaxial angle in the occipitocervical stabilization using an original construct: a retrospective study on 50 patients. Eur Spine J. 2009;18 Suppl 1(1):7-12.
[12] TAIGO I, TAKEO F, KOSHIRO K, et al. Postoperative increase in occiput–c2 angle negatively impacts subaxial lordosis after occipito–upper cervical posterior fusion surgery. Asian Spine J. 2016;10(4):744-747.
[13] YOSHIDA M, NEO M, FUJIBAYASHI S, et al. Upper-airway obstruction after short posterior occipitocervical fusion in a flexed position. Spine. 2007; 32(8): E267-270.
[14] MASANORI I , MASASHI N ,MITSURU T,et al. The O-C2 angle established at occipito- cervical fusion dictates the patient’s destiny in terms of postoperative dyspnea and/or dysphagia. Eur Spine J. 2014;23:328-336.
[15] SHESHADRI V , MOGA R , MANNINEN P , et al. Airway adverse events following posterior occipito-cervical spinal fusion. J Clin Neurosci. 2017; 39:124-129.
[16] NAGASHIMA S,NAGAE M,ARAI Y, et al. A new method of measuring the occipitocervical angle that could be applied as an intraoperative indicator during occipitocervical fusion. Clin Spine Surg. 2016;30(7):981-987.
[17] GROB D, FRAUENFELDER H, MANNION AF. The association between cervical spine curvature and neck pain. Eur Spine J. 2007;16(5): 669-678.
[18] GUO Q , NI B , YANG J , et al. Relation between alignments of upper and subaxial cervical spine: a radiological study. Arch Orthopa Trauma Surg. 2011; 131(6):857-862.
[19] PASSIAS PG , WANG S , KOZANEK M , et al. Relationship between the alignment of the occipitoaxial and subaxial cervical spine in patients with congenital atlantoxial dislocations. J Spinal Disord Tech. 2013;26(1):15-21.
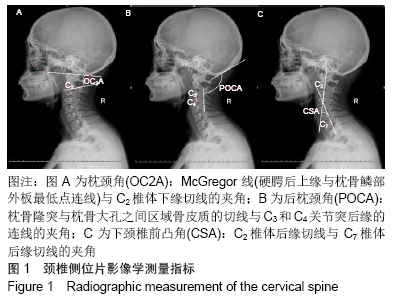
[20] RIEL RU , LEE MC , KIRKPATRICK JS . Measurement of a posterior occipitocervical fusion angle. J Spinal Disord Tech. 2010; 23(1):27-29.
[21] MAULUCCI CM, GHOBRIAL GM, SHARAN AD,et al. Correlation of posterior occipitocervical angle and surgical outcomes for occipitocervical fusion. Evid Based Spine Care J. 2014; 5(2):163-165.
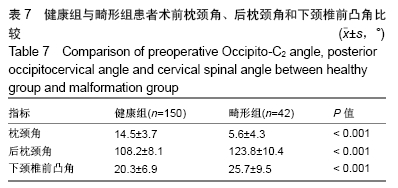
[22] 李广州,刘浩,丁琛,等. 后路枕颈融合术中联合应用后枕颈角和枕颈角调整枕颈固定角度的临床研究[J]. 中国修复重建外科杂志, 2019, 33(1):42-47.
[23] GORE D. Roentgenographic findings of the cervical spine in asymptomatic patients. Spine. 1986;11(6):521-524.
[24] FOERSTER O. Die leitungsbahnen des schmerzgefuhls und die chirurgische behandlung der schmerzustande. Berlin: Urban and Schwarzenberg,1927:266-267.
[25] SHEREKAR SK, YADAV YR, BASOOR AS, et al. Clinical implications of alignment of upper and lower cervical spine. Neurol India. 2006;54(3): 264-267.
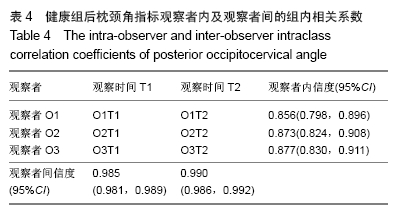
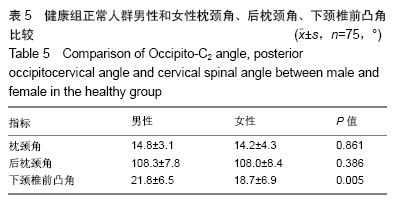
[26] 唐超,李广州,廖烨晖,等.150例健康成人枕颈角和后枕颈角影像参数测量及其临床意义[J].中国脊柱脊髓杂志,2018,28(3):239-244.
[27] 张鹏. 枕颈融合术后下颈椎曲度异常的生物力学和临床研究[D].上海:中国人民解放军海军军医大学,2018.
[28] KUNAKORNSAWAT S, PLUEMVITAYAPORN T, PRUTTIKUL P, et al. A new method for measurement of occipitocervical angle by occiput-C3 angle. Eur J Orthop Surg Traumatol. 2017;27(8): 1051-1056.
[29] WU X , QI Y , TAN M , et al. Incidence and risk factors for adjacent segment degeneration following occipitoaxial fusion for atlantoaxial instability in non-rheumatoid arthritis. Arch Orthop Trauma Surg. 2018; 138(7):921-927.
[30] GOEL A. Instability and basilar invigilation. J Craniovertebr Junction Spine. 2012;3(1): 1-2.
[31] MENEZES AH. Craniovertebral junction database analysis: incidence classification, presentation, and treatment algorithms. Childs Nerv Syst. 2008;24(10): 1101-1108.
[32] OGIHARA N, TAKAHASHI J, HIRABAYASHI H, et al. Surgical treatment of Klippel-Feil syndrome with basilar invigilation. Eur Spine J. 2013;22 Suppl (3): 1-8.
[33] SALUNKE P, SHARMA M, SODHI HB, et al. Congenital atlantoaxial dislocation: a dynamic process and role of facets in irreducibility: Clinical article. J Neurosurg Spine. 2011; 15(6): 678-685.
[34] TANG C, LI GZ, LIAO YH, et al. Importance of the occipitoaxial angle and posterior occipitocervical angle in occipitocervical fusion. Orthop Surg. 2019;11(6):1054-1063.
[35] GLASSMAN SD, BERVEN S, BRIDWELL K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976). 2005; 30(6):682-688.
[36] BERJANO P, BASSANI R, CASERO G, et al. Failures and revisions in surgery for sagittal imbalance: analysis of factors influencing failure. Eur Spine J. 2013;22 Suppl 6:S853-858.
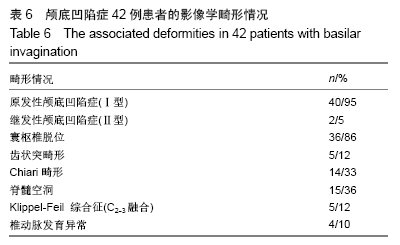
[37] 孟阳,刘浩,戎鑫,等.颅底凹陷症合并寰枢椎脱位患者枕颈角与下颈椎曲度的关系[J].中国脊柱脊髓杂志,2017,27(1):25-30.
|