中国组织工程研究 ›› 2020, Vol. 24 ›› Issue (21): 3341-3346.doi: 10.3969/j.issn.2095-4344.2703
• 骨与关节图像与影像 bone and joint imaging • 上一篇 下一篇
任务态fMRI对脊髓型颈椎病严重程度及手术预后的评价
宋彦澄1,2,康立清2,申沧海3,刘凤海2,冯永健3
1天津医科大学沧州市中心医院教学医院,河北省沧州市 061000;沧州市中心医院,2磁共振成像科,3骨四科,河北省沧州市 061000
Application of task-state fMRI in evaluating disease severity and prognosis of cervical spondylotic myelopathy
Song Yancheng1, 2, Kang Liqing2, Shen Canghai3, Liu Fenghai2, Feng Yongjian3#br#
- 1Teaching Hospital of Cangzhou Central Hospital, Tianjin Medical University, Cangzhou 061000, Hebei Province, China; 2Department of MRI, 3Four Department of Orthopedic Surgery, Cangzhou Central Hospital, Cangzhou 061000, Hebei Province, China
摘要:
文题释义:
血氧水平依赖功能磁共振:是一种非侵入性的检测方法。该技术依赖于脑血流和神经元激活的耦合,当大脑的某个区域处于活动状态时,流向该区域的血液会随之增加,超过了代谢需求时,顺磁性去氧血红蛋白浓度会相对下降,这一效应会减弱局部磁场的不均匀性,从而显示出成像信号的差异。
皮质重构:脊髓受到损伤后患者会出现脑皮质功能活动的改变。相对于正常健康人群,这种脑皮质活动的异常,类似于一种特殊的激活区域空间移位,被称之为皮质重构。神经组织的可塑性是脊髓损伤后脑皮质能够发生重构的重要原因。
背景:血氧水平依赖功能磁共振(BOLD-fMRI)通过检测大脑功能区活动时血流变化而获得脑功能改变的客观信息。以往关于脊髓型颈椎病的任务态fMRI研究能够观察到患者感觉和运动皮质功能的重构。
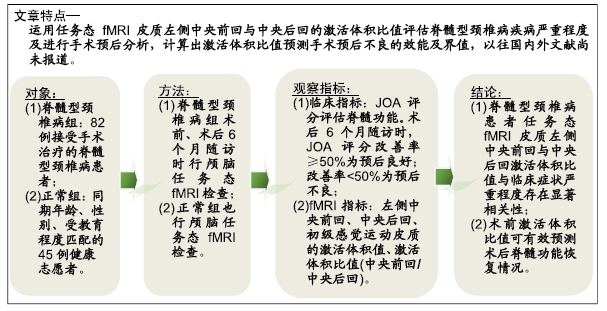
目的:运用任务态fMRI分析脊髓型颈椎病患者皮质激活的变化程度与临床症状严重程度及手术预后之间的关系。
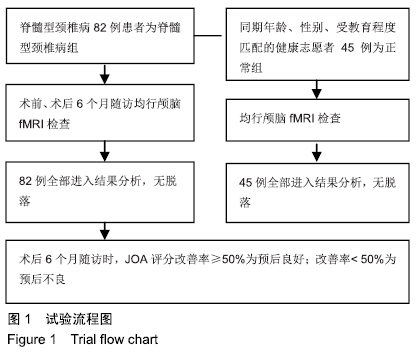
方法:2018年1月至2019年1月收集行颈椎后路减压手术治疗的脊髓型颈椎病患者82例(脊髓型颈椎病组)及健康志愿者45名(正常组)。所有对象均行颅脑fMRI扫描,动作任务均为右手对指任务。采用日本骨科学会(JOA)评分评估患者脊髓功能,术后6个月随访时将JOA评分改善率< 50%定义为手术预后不良。
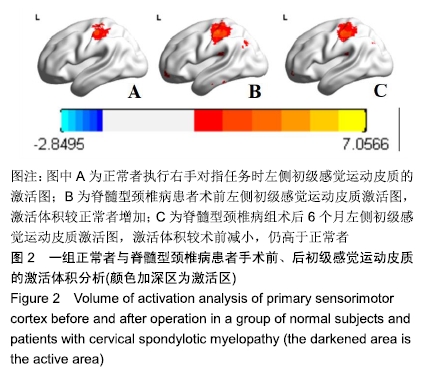
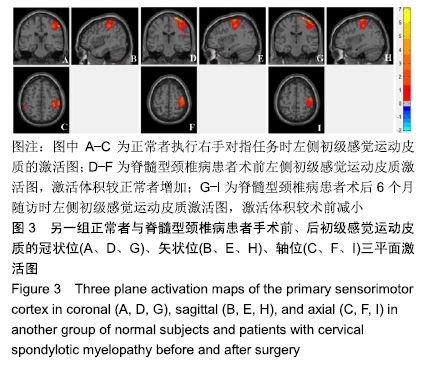
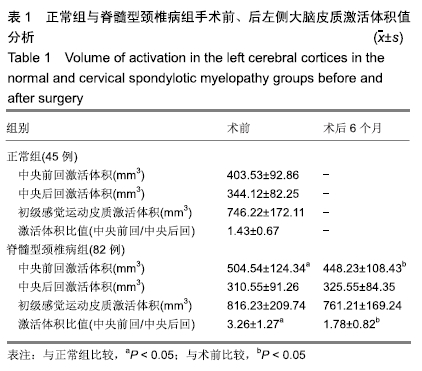
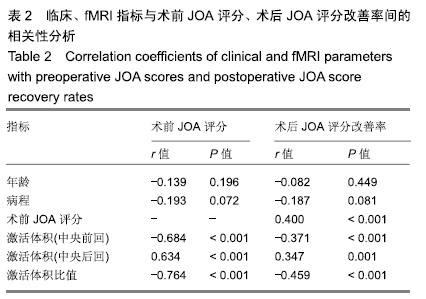
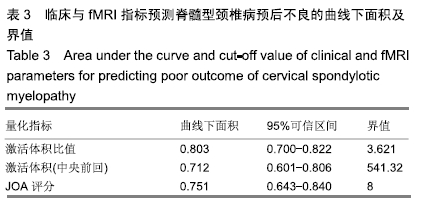
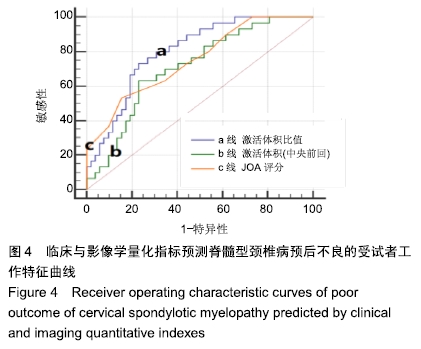
结果与结论:①脊髓型颈椎病组术后JOA评分较术前显著改善(P < 0.05);②脊髓型颈椎病组术前左侧中央前回的激活体积值较正常组显著升高(P < 0.05),左侧中央后回的激活体积值与正常组差异无显著性意义(P > 0.05);脊髓型颈椎病组术前左侧激活体积比值(中央前回/中央后回)较正常组显著升高(P < 0.05);③术后6个月随访时,脊髓型颈椎病组左侧中央前回的激活体积值较术前显著减低(P < 0.05),左侧中央后回的激活体积值与术前差异无显著性意义(P > 0.05),左侧激活体积比值较术前显著降低(P < 0.05);④相关性分析显示左侧中央前回、中央后回的激活体积值、激活体积比值与术前JOA评分、术后JOA评分改善率间均具有显著相关性(P < 0.05)。激活体积比值与术前JOA评分、术后改善率的相关系数绝对值最大;⑤受试者工作特征曲线分析发现术前激活体积比值预测预后不良的曲线下面积为0.803,界值为3.621;术前JOA评分预测预后不良的曲线下面积为0.751,界值为8;激活体积比值的预测效能高于JOA评分;⑥结果表明,脊髓型颈椎病患者任务态fMRI皮质左侧中央前回与中央后回的激活体积比值与临床症状严重程度(JOA评分)存在显著负相关。术前激活体积比值可有效预测脊髓型颈椎病患者术后脊髓功能恢复情况。
ORCID: 0000-0002-9156-0702(宋彦澄)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号: