中国组织工程研究 ›› 2018, Vol. 22 ›› Issue (15): 2315-2320.doi: 10.3969/j.issn.2095-4344.0759
• 人工假体 artificial prosthesis • 上一篇 下一篇
高龄慢性肾功能不全股骨近端骨折生物型人工股骨头置换的中短期随访
左威敏1,杨 龙2,王建吉2,叶 川2
- 1贵州医科大学,贵州省贵阳市 550004;2贵州医科大学附属医院骨外科,贵州省贵阳市 550004
Middle- and short-term follow-up of biological artificial femoral head replacement in elderly patients with proximal femoral fracture of chronic renal disease
Zuo Wei-min1, Yang Long2, Wang Jian-ji2, Ye Chuan2
- 1Guizhou Medical University, Guiyang 550004, Guizhou Province, China; 2Department of Orthopedic Surgery, Affiliated Hospital of Guizhou Medical University, Guiyang 550004, Guizhou Province, China
摘要:
文章快速阅读:
.jpg)
文题释义:
生物型假体:指假体表面具有微孔结构,可以通过骨长入实现假体与骨的良好固定,具有良好的远期固定效果。
高龄慢性肾功能不全股骨近端骨折:因慢性肾功能不全一般病史较长,晚期尿毒症患者有长期血液透析或者腹膜透析病史,伴有不同程度的贫血及营养不良,部分患者合并高钾血症及其他内科疾病,一般认为此类患者手术风险及术后并发症发生率增高。且此类患者往往伴有严重骨质疏松,内固定容易出现把持力不足,术后容易导致内固定松动、头颈螺钉切割等并发症而导致手术失败,且内固定无法实现早期下床活动,股骨颈骨折患者后期有并发股骨头坏死的风险。
摘要
背景:股骨近端骨折为老年人常见骨折,生物型人工股骨头置换是主要外科治疗方法之一,但是对伴有慢性肾功能不全的患者,其手术的安全性及修复效果报道结果差异很大。
目的:分析高龄慢性肾功能不全股骨近端骨折患者进行生物型人工股骨头置换的中短期疗效。
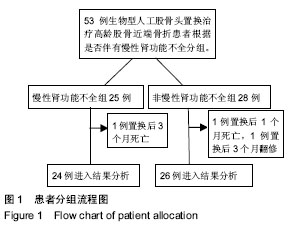
方法:纳入生物型人工股骨头置换治疗高龄(75岁及以上)股骨近端骨折患者53例,根据肾功能情况分为2组,慢性肾功能不全组25例,非慢性肾功能不全组28例。对比2组患者手术时间、术中出血量、输血量、术后24 h引流量、部分及完全负重时间、住院时间、住院费用以及并发症发生情况,比较随访时2组患者的髋关节功能Harris评分、双能X射线骨密度值、假体松动、假体周围骨溶解情况及假体生存率。
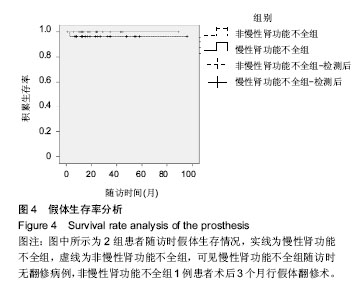
结果与结论:①非慢性肾功能不全组1例患者置换后1个月死于呼吸衰竭,1例置换后3个月进行了翻修手术;慢性肾功能不全组1例置换后3个月死于心肺功能衰竭。2组其余患者完成了1-8年的随访,修复效果均满意;②慢性肾功能不全组及非慢性肾功能不全组置换后6个月髋关节功能Harris评分优良率分别为83%及85%,差异无显著性意义(P > 0.05);③2组患者的手术时间、出血量、术后24 h引流量、部分及完全负重时间、双能X射线骨密度值差异均无显著性意义,但慢性肾功能不全组输血量更大,与非慢性肾功能不全组相比,住院时间长,住院费用多;④2组患者术后随访时均有不同程度的假体周围骨溶解,但无明显假体松动;非慢性肾功能不全组1例患者因反复假体脱位最终翻修,慢性肾功能不全组及非慢性肾功能不全组假体生存率分别为100%及96%,差异无显著性意义(P > 0.05);⑤结果提示,对于合并慢性肾功能不全的高龄股骨近端骨折患者,经过周密的术前准备,应用生物型人工股骨头置换可取得良好的修复效果,患者肢体功能改善明显。
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
ORCID: 0000-0001-5690-6416(左威敏)
中图分类号:

.jpg)