[1] VERHAGEN AP, VAN MIDDELKOOP M, RUBINSTEIN SM, et al. Effect of various kinds of cervical spinal surgery on clinical outcomes: a systematic review and meta-analysis. Pain. 2013;154(11):2388-2396.
[2] SMITH GW, ROBINSON RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-a(3):607-624.
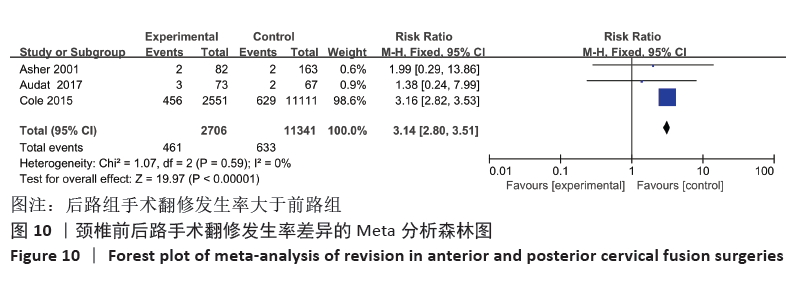
[3] VEERAVAGU A, COLE T, JIANG B, et al. Revision rates and complication incidence in single- and multilevel anterior cervical discectomy and fusion procedures: an administrative database study. Spine J. 2014;14(7):1125-1131.
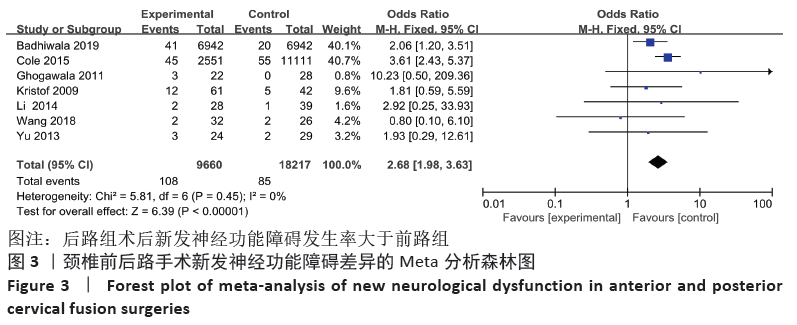
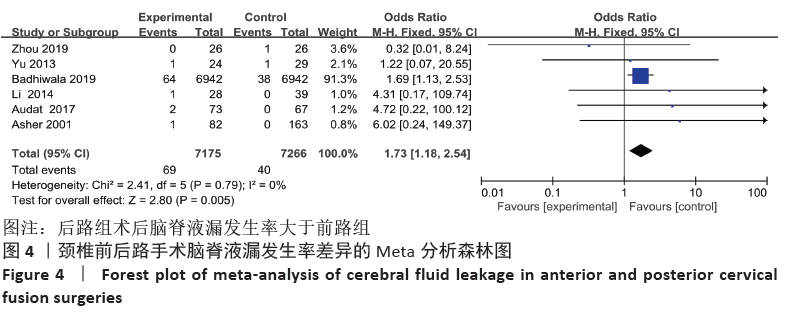
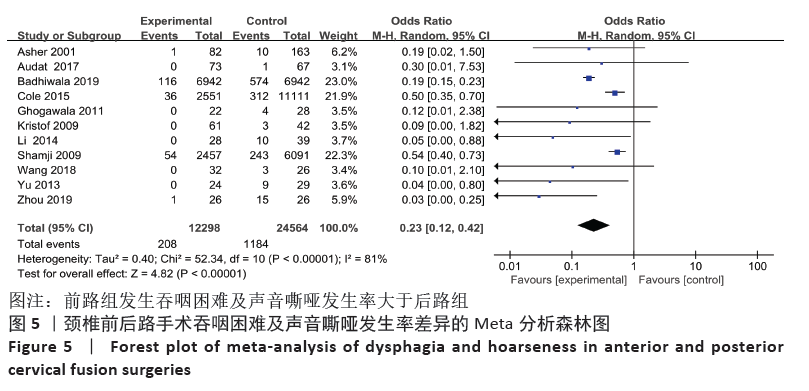
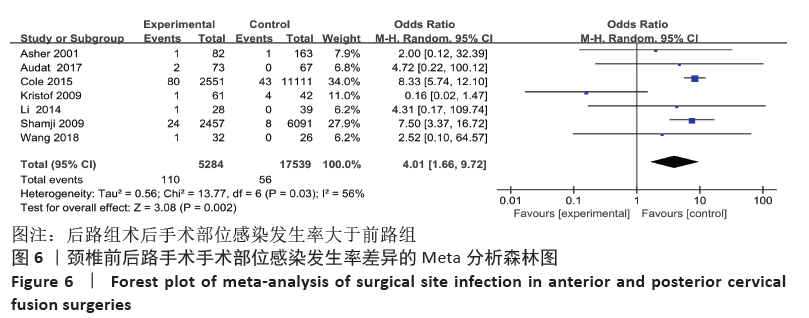
[4] CURRIER BL. Neurological complications of cervical spine surgery: C5 palsy and intraoperative monitoring. Spine. 2012; 37(5):E328-E334.
[5] WOODS BI, HOHL J, LEE J, et al. Laminoplasty versus laminectomy and fusion for multilevel cervical spondylotic myelopathy. Clin Orthop Related Res. 2011; 469(3):688-695.
[6] YOSHII T, EGAWA S, CHIKUDA H, et al. Comparison of anterior decompression with fusion and posterior decompression with fusion for cervical spondylotic myelopathy-A systematic review and meta-analysis. J Orthop Sci. 2020;25(6):938-945.
[7] CHEN Z, LIU B, DONG J, et al. A comparison of the anterior approach and the posterior approach in treating multilevel cervical myelopathy: a meta-analysis. Clin Spine Surg. 2017;30(2):65-76.
[8] LUO J, CAO K, HUANG S, et al. Comparison of anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy. Eur Spine J. 2015;24(8):1621-1630.
[9] XU L, SUN H, LI Z, et al. Anterior cervical discectomy and fusion versus posterior laminoplasty for multilevel cervical myelopathy: a meta-analysis. Int J Surg. 2017;48:247-253.
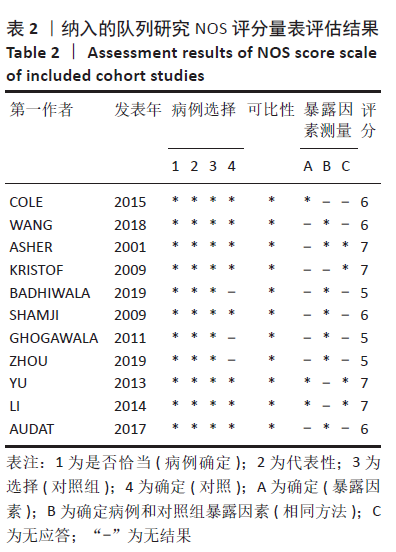
[10] 曾宪涛,包翠萍,曹世义,等.Meta分析系列之三:随机对照试验的质量评价工具[J].中国循证心血管医学杂志,2012, 4(3):183-185.
[11] STANG A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010; 25(9):603-605.
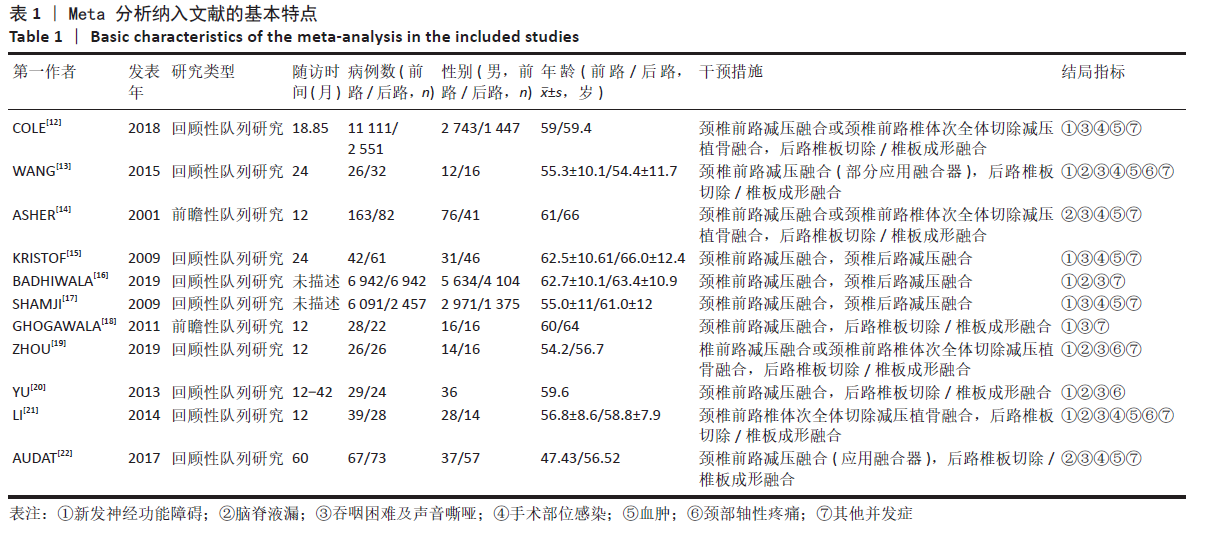
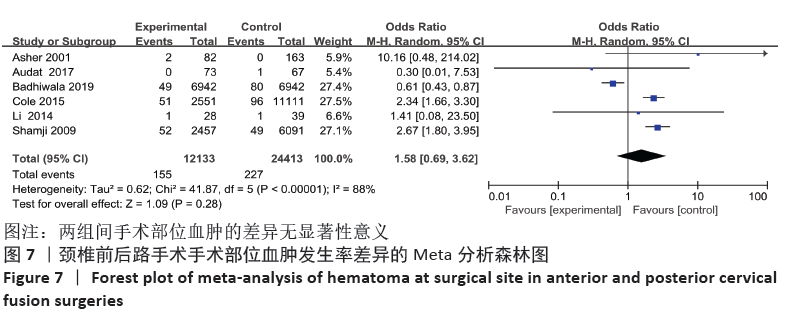
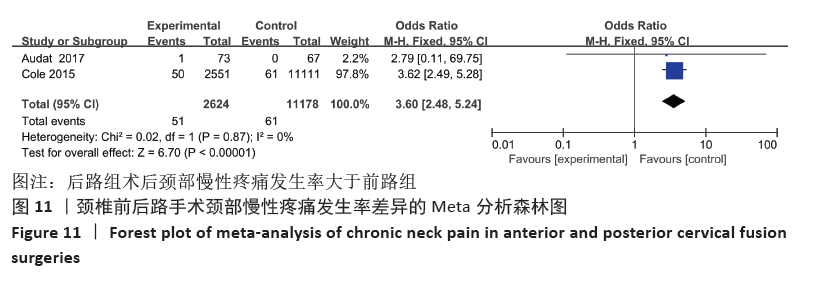
[12] COLE T, VEERAVAGU A, ZHANG M, et al. Anterior versus posterior approach for multilevel degenerative cervical disease: a retrospective propensity score-matched study of the marketscan database. Spine. 2015;40(13):1033-1038.
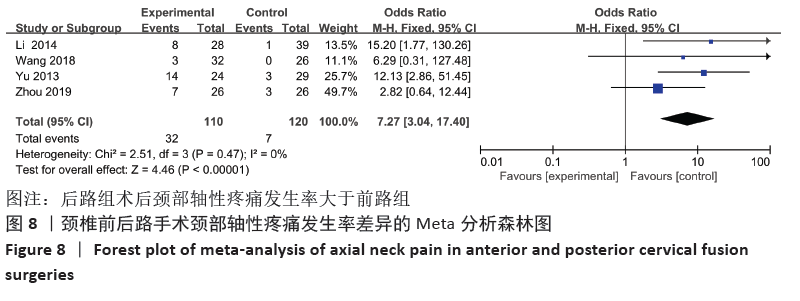
[13] WANG B, Lü G, KUANG L. Anterior cervical discectomy and fusion with stand-alone anchored cages versus posterior laminectomy and fusion for four-level cervical spondylotic myelopathy: a retrospective study with 2-year follow-up. BMC Musculoskelet Disord. 2018;19(1):216.
[14] ASHER AL, DEVIN CJ, KEREZOUDIS P, et al. Comparison of outcomes following anterior vs posterior fusion surgery for patients with degenerative cervical myelopathy: an analysis from quality outcomes database. Neurosurgery. 2019;84(4):919-926.
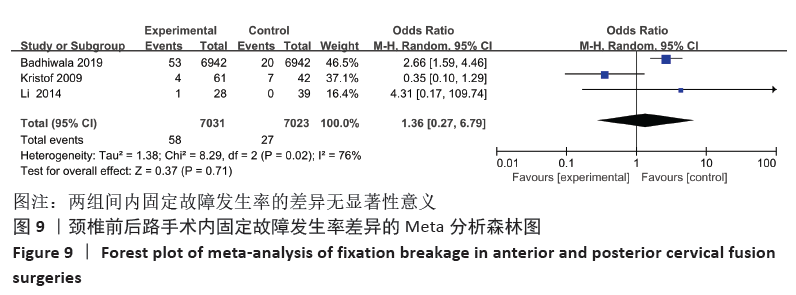
[15] KRISTOF RA, KIEFER T, THUDIUM M, et al. Comparison of ventral corpectomy and plate-screw-instrumented fusion with dorsal laminectomy and rod-screw-instrumented fusion for treatment of at least two vertebral-level spondylotic cervical myelopathy. Eur Spine J. 2009;18(12): 1951-1956.
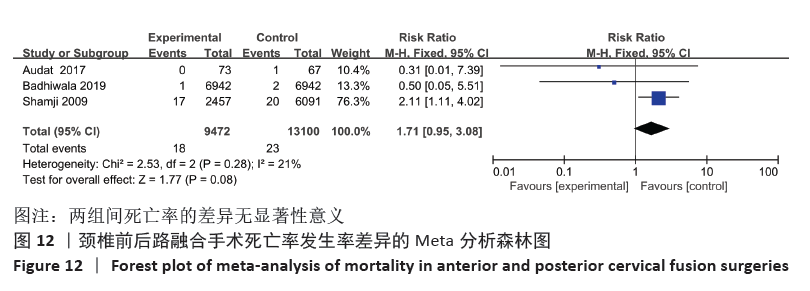
[16] BADHIWALA JH, ELLENBOGEN Y, KHAN O, et al. Comparison of the inpatient complications and health care costs of anterior versus posterior cervical decompression and fusion in patients with multilevel degenerative cervical myelopathy: a retrospective propensity score-matched analysis. World Neurosurg. 2020;134:e112-e119.
[17] SHAMJI MF, COOK C, PIETROBON R, et al. Impact of surgical approach on complications and resource utilization of cervical spine fusion: a nationwide perspective to the surgical treatment of diffuse cervical spondylosis. Spine J. 2009; 9(1):31-38.
[18] GHOGAWALA Z, BROOK M, BENZEL E C, et al. Comparative effectiveness of ventral versus dorsal surgery for cervical spondylotic myelopathy. Eur Spine J. 2010; 19(6):1054.
[19] ZHOU C, LIU C, PANCHAL RR, et al. Modified expansive laminoplasty and fusion compared with anterior cervical surgeries in treating four-level cervical spondylotic myelopathy. J Int Med Res. 2019;47(6):2413-2423.
[20] SHUNZHI Y, ZHONGHAI L, FENGNING L, et al. Surgical management of 4-level cervical spondylotic myelopathy. Orthopedics. 2013; 36(5):e613-e620.
[21] LI Z, GUO Z, HOU S, et al. Segmental anterior cervical corpectomy and fusion with preservation of middle vertebrae in the surgical management of 4-level cervical spondylotic myelopathy. Eur Spine J. 2014; 23(7):1472-1479.
[22] AUDAT ZA, FAWAREH MD, RADYDEH AM, et al. Anterior versus posterior approach to treat cervical spondylotic myelopathy, clinical and radiological results with long period of follow-up. SAGE Open Med. 2018;6:2050312118766199.
[23] WITWER BP, TROST GR. Cervical spondylosis: ventral or dorsal surgery. Neurosurgery. 2007;60(1 Supp1 1):S130-S136.
[24] AL EISSA S, KONBAZ F, ALDEGHAITHER S, et al. Anterior cervical discectomy and fusion complications and thirty-day mortality and morbidity. Cureus. 2020;12(4):e7643.
[25] CHEN Q, QIN M, CHEN F, et al. Comparison of outcomes between anterior cervical decompression and fusion and posterior laminoplasty in the treatment of 4-level cervical spondylotic myelopathy. World Neurosurg. 2019;125:e341-e347.
[26] DEBONO B, CORNIOLA MV, PIETTON R, et al. Benefits of enhanced recovery after surgery for fusion in degenerative spine surgery: impact on outcome, length of stay, and patient satisfaction. Neurosurgical Focus. 2019;46(4):E6.
[27] REN J, LI R, ZHU K, et al. Biomechanical comparison of percutaneous posterior endoscopic cervical discectomy and anterior cervical decompression and fusion on the treatment of cervical spondylotic radiculopathy. J Orthop Surg Res. 2019; 14(1):71.
[28] SALZMANN SN, DERMAN PB, LAMPE LP, et al. Cervical spinal fusion: 16-year trends in epidemiology, indications, and in-hospital outcomes by surgical approach. World Neurosurg. 2018;113:e280-e295.
[29] FEHLINGS MG, BARRY S, KOPJAR B, et al. Anterior versus posterior surgical approaches to treat cervical spondylotic myelopathy: outcomes of the prospective multicenter AOSpine North America CSM study in 264 patients. Spine. 2013; 38(26):2247-2252.
[30] LIN D, ZHAI W, LIAN K, et al. Anterior versus posterior approach for four-level cervical spondylotic myelopathy. Orthopedics. 2013; 36(11):e1431-1436.
[31] YOUSSEF JA, HEINER AD, MONTGOMERY JR, et al. Outcomes of posterior cervical fusion and decompression: a systematic review and meta-analysis. Spine J. 2019;19(10): 1714-1729.
[32] PAN FM, WANG SJ, MA B, et al. C5 nerve root palsy after posterior cervical spine surgery. Journal of orthopaedic surgery (Hong Kong). 2017;25(1):2309499016684502.
[33] ZHU N, XIE D, DENG QY, et al. Comment on Zhu et al. entitled ‘‘Anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy: a systemic review and meta-analysis’’. Eur Spine J. 2014;23(2):486.
[34] KOMOTAR RJ, MOCCO J, KAISER MG. Surgical management of cervical myelopathy: indications and techniques for laminectomy and fusion. Spine J. 2006;6(6 Suppl):
252s-267s.
[35] NAKASHIMA H, YUKAWA Y, IMAGAMA S, et al. Complications of cervical pedicle screw fixation for nontraumatic lesions: a multicenter study of 84 patients. J Neurosurg Spine. 2012;16(3):238-247.
[36] GU Y, CAO P, GAO R, et al. Incidence and risk factors of C5 palsy following posterior cervical decompression: a systematic review. PLoS One. 2014;9(8):e101933.
[37] KATSUMI K, YAMAZAKI A, WATANABE K, et al. Can prophylactic bilateral C4/C5 foraminotomy prevent postoperative C5 palsy after open-door laminoplasty?: a prospective study. Spine. 2012;37(9): 748-754.
[38] WADA E, SUZUKI S, KANAZAWA A, et al. Subtotal corpectomy versus laminoplasty for multilevel cervical spondylotic myelopathy: a long-term follow-up study over 10 years. Spine. 2001;26(13):1443-1447;discussion 8.
[39] WANG SJ, JIANG SD, JIANG LS, et al. Axial pain after posterior cervical spine surgery: a systematic review. Eur Spine J. 2011;20(2):185-194.
[40] NAKAMA S, NITANAI K, OOHASHI Y, et al. Cervical muscle strength after laminoplasty. J Orthop Sci. 2003;8(1):36-40.
[41] SILVERMAN JL, RODRIQUEZ AA, AGRE JC. Quantitative cervical flexor strength in healthy subjects and in subjects with mechanical neck pain. Arch Phys Med Rehabil. 1991;72(9):679-681.
[42] CAMPBELL PG, YADLA S, MALONE J, et al. Early complications related to approach in cervical spine surgery: single-center prospective study. World Neurosurgery. 2010;74(2-3):363-368.
[43] 石云志,刘泉.长节段颈椎后纵韧带骨化症修复:后路椎板切除植骨内固定与前路椎体次全切除减压的比较[J].中国组织工程研究,2014,18(53):8601-8606.
[44] ROSENTHAL BD, NAIR R, HSU WK, et al. Dysphagia and dysphonia assessment tools after anterior cervical spine surgery. Clin Spine Surg. 2016;29(9):363-367.
[45] 严妹,胡学昱,王倩.前路与后路减压融合术治疗颈椎后纵韧带骨化症的效果比较及术后1年预后的影响因素分析[J].中国医药,2019,14(6):909-913.
[46] CHE W, LI RY, DONG J. Progress in diagnosis and treatment of cervical postoperative infection. Orthop Surg. 2011;3(3):152-157.
[47] BARNES M, LIEW S. The incidence of infection after posterior cervical spine surgery: a 10 year review. Global Spine J. 2012;2(1):3-6.
[48] NASSER R, KOSTY JA, SHAH S, et al. Risk Factors and Prevention of Surgical Site Infections Following Spinal Procedures. Global Spine J. 2018;8(4 Suppl):44s-48s. |