中国组织工程研究 ›› 2021, Vol. 25 ›› Issue (4): 499-503.doi: 10.3969/j.issn.2095-4344.2359
• 组织工程口腔材料 tissue-engineered oral materials • 上一篇 下一篇
不同生物活性支架治疗年轻恒牙再生牙髓活力的比较
李文静,李浩渤,刘从娜,程东梅,陈惠珍,张志勇
- 河北医科大学第二医院口腔内科,河北省石家庄市 050000
Comparison of different bioactive scaffolds in the treatment of regenerative pulp of young permanent teeth
Li Wenjing, Li Haobo, Liu Congna, Cheng Dongmei, Chen Huizhen, Zhang Zhiyong
- Department of Oral Medicine, Second Hospital of Hebei Medical University, Shijiazhuang 050000, Hebei Province, China
摘要:

文题释义:
再生性牙髓治疗:年轻恒压由于受外力损伤或牙髓炎可导致牙髓坏死,导致牙齿发育中断,根尖不能闭合,若直接填充或根管治疗可导致牙齿损坏脱离。再生性牙髓治疗可以对新鲜的损伤牙髓进行一定程度的暂时功能替代、诱导,进而促进根管继续发育,实现根尖孔闭合,其中关键的操作是选择合适的支架覆盖牙髓。
根尖孔封闭:正常情况下发育完成的牙根尖孔是封闭的,但年轻恒压受损后处理不当会导致发育中断,根尖孔无法封闭,导致牙齿不完整、不稳定,容易破碎脱离。通过再生性牙髓治疗可促进根尖继续发育,实现封闭。
背景:再生性牙髓治疗具有生物相容性好、牙根发育完善、牙髓活力保存率高等优点,其血管再生过程中需要借助支架以维持干细胞的生存和血管再生。
目的:分析不同生物活性支架应用于年轻恒牙再生性牙髓治疗的效果。
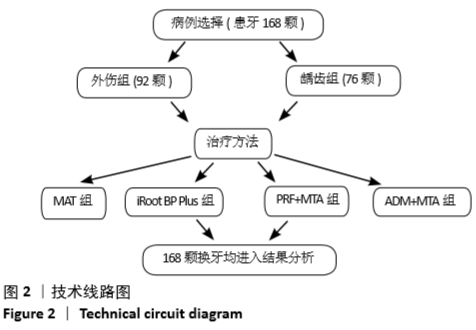
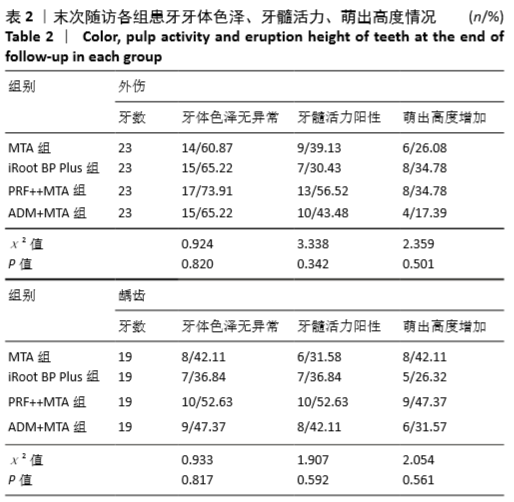
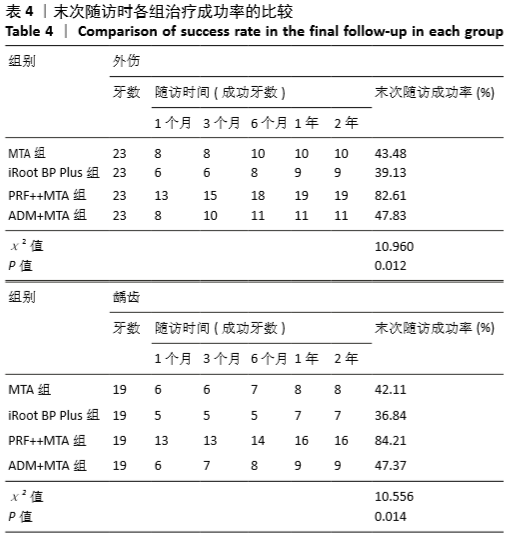
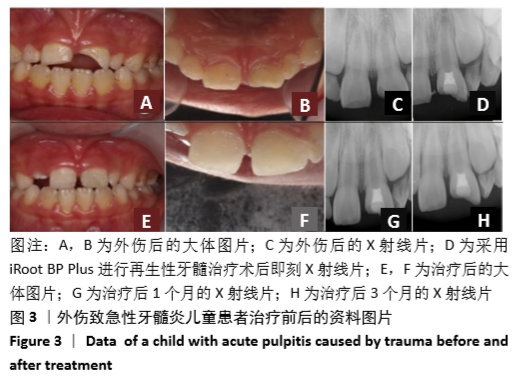
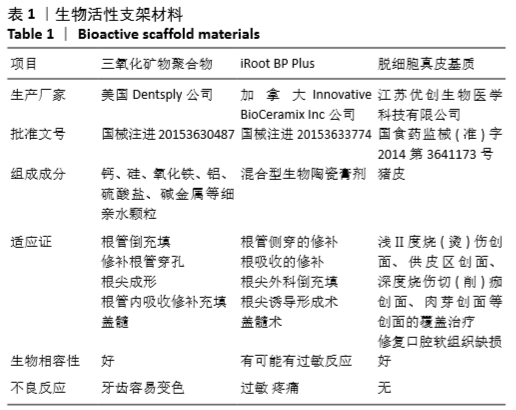
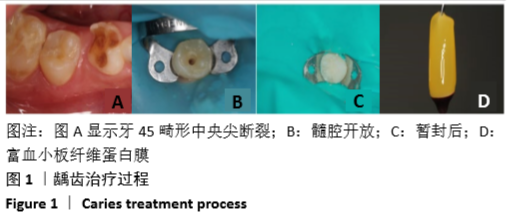
方法:选择2016年6月至2018年6月河北医科大学第二医院收治的急性牙髓炎患者160例(患牙168颗),年龄8-16岁,按病因分为外伤组(n=92)和龋齿组(n=76),每组内分别使用4种支架进行再生性牙髓治疗,4种支架分别为三氧化矿物聚合物(MTA组)、iRoot BP Plus、自体富血小板纤维蛋白联合三氧化矿物聚合物(PRF+MTA组)、脱细胞真皮基质联合三氧化矿物聚合物(ADM+MTA组)。记录1,3,6,12,24个月患牙的牙体色泽、牙髓活力、萌出高度,采用X射线摄像比较根管长度、根管壁厚度、根尖周暗影及根尖孔封闭情况,统计成功率。研究获得河北医科大学第二医院伦理委员会批准。
结果与结论:①外伤组末次随访时,4种支架组间的牙体色泽、牙髓活力、萌出高度比较差异无显著性意义(P > 0.05),4种支架组间的根管长度、根管壁厚度、根尖周暗影、根尖孔封闭情况比较差异有显著性意义(P < 0.05),其中PRF+MTA组效果最好;②龋齿组末次随访时,4种支架组间的牙体色泽、牙髓活力、萌出高度比较差异无显著性意义(P > 0.05),4种支架组间的根管长度、根管壁厚度、根尖周暗影、根尖孔封闭情况比较差异有显著性意义(P < 0.05),其中PRF+MTA组效果最好;③无论是外伤组还是龋齿组,4种支架组间的治疗成功率比较差异有显著性意义(P < 0.05),其中以PRF+MTA组最高;④结果表明,自体富血小板纤维蛋白联合三氧化矿物聚合物在年轻恒牙再生性牙髓治疗中有优秀的生物诱导性,较其他支架能更好地保存牙髓活力,诱导年轻恒牙牙根形成,提高治疗成功率。
https://orcid.org/0000-0002-6997-1927 (李文静)
中国组织工程研究杂志出版内容重点:生物材料;骨生物材料; 口腔生物材料; 纳米材料; 缓释材料; 材料相容性;组织工程
中图分类号: