[1] 粟迎春.经皮椎体成形术和经皮椎体后凸成形术治疗骨质疏松性椎体压缩骨折的疗效[J].实用医学杂志,2017,33(2):273-275.
[2] WARDLAW D, CUMMINGS SR, MEIRHAEGHE JV, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE):a randomised controlled trial. Lancet. 2009;373(9668):1016-1024.
[3] 王真,吕金捍,万宁军,等.老年骨质疏松椎体骨折PVP术后骨水泥渗漏的相关危险因素[J].中国老年学杂志,2017,37(23):5890-5892.
[4] 夏维波,章振林,林华,等.原发性骨质疏松症诊疗指南(2017)[J].中国骨质疏松杂志,2019,25(3):281-309.
[5] YEOM JS, KIM WJ, CHOY WS, et al. Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J Bone Joint Surg Br. 2003;85(1):83-89.
[6] 于学忠,刘健健,齐国宝,等.PVP治疗骨质疏松性椎体压缩骨折骨水泥渗漏原因分析[J].中国骨与关节损伤杂志,2017,32(11):1176-1177.
[7] HATZANTONIS C, CZYZ M, PYZIK R, et al. Intracardiac bone cement embolism as a complication of vertebroplasty: management strategy. Eur Spine J. 2017; 26(12):3199-3205.
[8] BARAKAT AS, OWAIS T, ALHASHASH M, et al. Presentation and management of symptomatic central bone cement embolization. Eur Spine J. 2018;27(10):2584-2592.
[9] 姚方超,吴玉杰,王惠东,等.改良穿刺套管在经皮椎体成形术中预防骨水泥渗漏的研究[J].中华创伤骨科杂志,2019(12):1029-1035.
[10] 王华锋,叶小伟,周福山,等.PVP术后有症状椎管内骨水泥渗漏的诊治并文献回顾[J].中国骨与关节损伤杂志,2019,34(5):499-501.
[11] Zhu SY, Zhong ZM, Wu Q, et al. Risk factors for bone cement leakage in percutaneous vertebroplasty: a retrospective study of four hundred and eighty five patients. Int Orthop. 2016;40(6):1205-1210.
[12] HSIEH MK, KAO FC, CHIU PY, et al. Risk factors of neurological deficit and pulmonary cement embolism after percutaneous vertebroplasty. J Orthop Surg Res. 2019;14(1):406.
[13] 崔利宾,唐本强,王彦辉,等.年龄≥80岁骨质疏松性椎体压缩骨折患者经皮椎体成形术骨水泥渗漏的危险因素分析[J].中国脊柱脊髓杂志,2020, 30(6):530-538.
[14] 文豪,刘元,张柯,等.椎体强化术骨水泥渗漏并发症及预防的研究进展[J].中国矫形外科杂志,2019,27(12):1111-1115.
[15] WANG M, JIN Q. High-viscosity bone cement for vertebral compression fractures: a prospective study on intravertebral diffusion and leakage of bone cement. BMC Musculoskelet Disord. 2020;21(1):589.
[16] 刘洋,李明辉,梅红军.经皮椎体成形术后骨水泥渗漏的回顾性分析及预防策略[J].中国骨质疏松杂志,2013,19(4):375-380.
[17] 郑毓嵩,张勇,林金丁,等.椎体成形术骨水泥渗漏的相关危险因素分析[J].中华创伤杂志,2015,31(4):312-316.
[18] MCCALL T, COLE C, DAILEY A. Vertebroplasty and kyphoplasty: a comparative review of efficacy and adverse events. Curr Rev Musculoskelet Med. 2008;1(1):17-23.
[19] ZHAN Y, JIANG J, LIAO H, et al. Risk Factors for Cement Leakage After Vertebroplasty or Kyphoplasty: A Meta-Analysis of Published Evidence. World Neurosurg. 2017;101:633-642.
[20] 王真,吕金捍,万宁军,等.老年骨质疏松椎体骨折PVP术后骨水泥渗漏的相关危险因素[J].中国老年学杂志,2017,37(23):5890-5892.
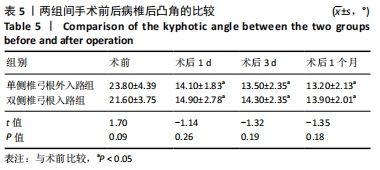
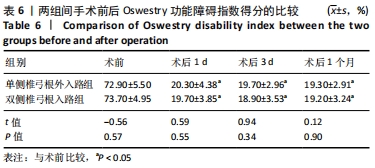
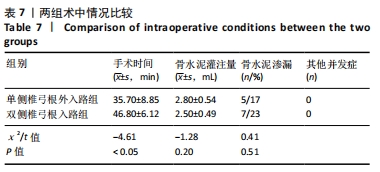
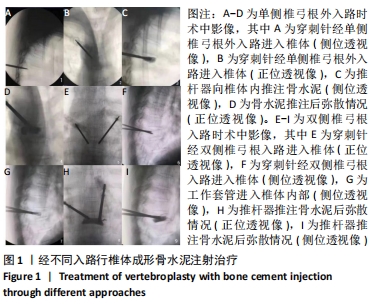
[21] 张志伟,李利,黄兹谕,等.单、双侧椎弓根入路及单侧椎弓根外入路椎体成形治疗胸腰段椎体压缩性骨折:骨水泥灌注量与渗漏率[J].中国组织工程研究,2020,24(9):1353-1358.
[22] 韦学昌,刘帅,张豪伟,等.单侧椎弓根外入路与双侧椎弓根入路PVP治疗骨质疏松性椎体压缩骨折的临床对比研究[J].现代诊断与治疗,2019,30(2): 276-277.
[23] 金桥,牛志军.单侧椎弓根外穿刺PKP术治疗高位胸椎骨质疏松压缩性骨折的疗效[J].实用骨科杂志,2020,26(10):914-917.
[24] ZHANG K, SHE J, ZHU Y, et al. Risk factors of postoperative bone cement leakage on osteoporotic vertebral compression fracture: a retrospective study. J Orthop Surg Res. 2021;16(1):183.
[25] 薛广,杨新明,张瑛.超前镇痛在经皮椎体后凸成形术治疗老年骨质疏松性椎体压缩骨折术中的镇痛效果及安全性[J].中华损伤与修复杂志(电子版), 2020,15(5):383-388.
[26] 贾川,黎俊,赵洪,等.单侧经横突-椎弓根入路与双侧经椎弓根入路经皮椎体成形术治疗重度骨质疏松性椎体压缩性骨折合并脊柱侧弯的比较研究[J].中医正骨,2018,30(12):23-29.
[27] 罗同青,谢湘涛,胡朝晖.单侧椎弓根外侧入路椎体成形术治疗骨质疏松性压缩骨折的临床研究[J]. 中国现代手术学杂志,2013,17(2):130-135.
[28] 徐建彪,王占长,梁宁,等.单侧椎弓根外入路与椎弓根入路PVP治疗胸腰段骨质疏松性椎体压缩骨折[J]. 中国骨与关节损伤杂志,2020,35(5):483-485.
[29] 周峰,杨惠林,干旻峰,等.单侧椎弓根外途径椎体后凸成形术治疗胸椎骨质疏松性压缩性骨折[J].苏州大学学报(医学版),2010,30(6):1129-1131+1155.
[30] 戈朝晖,赵浩宁,詹学华,等.单侧椎弓根外入路椎体后凸成形术治疗胸椎骨质疏松性椎体压缩骨折38例[J].中国组织工程研究与临床康复,2009, 13(48):9536-9540.
|