中国组织工程研究 ›› 2020, Vol. 24 ›› Issue (33): 5277-5282.doi: 10.3969/j.issn.2095-4344.2888
• 人工假体 artificial prosthesis • 上一篇 下一篇
人工全膝关节置换治疗膝关节外翻畸形
张朝鸣1,林天烨2,陈雷雷3,杨 鹏3,徐景利2,陈镇秋3,何 伟3,张庆文3
1广州中医药大学附属佛山中医院,广东省佛山市 528000;2广州中医药大学第一临床医学院,广东省广州市 510000;3广州中医药大学第一附属医院关节骨科,广东省广州市 510000
Total knee arthroplasty in the treatment of knee valgus deformity
Zhang Zhaoming1, Lin Tianye2, Chen Leilei3, Yang Peng3, Xu Jingli2, Chen Zhenqiu3, He Wei3, Zhang Qingwen3
1Foshan Hospital of TCM Affiliated to Guangzhou University of Chinese Medicine; 2First Clinical Medical College of Guangzhou University of Chinese Medicine; 3Department of Joint Orthopedics, the First Affiliated Hospital of Guangzhou University of Chinese Medicine
摘要:
文题释义:
膝关节外翻畸形:也称为X型腿,指两足并立,当两侧膝关节紧靠时而双足内踝无法靠拢。是类风湿、膝关节退行性变、膝关节发育不良、胫骨平台骨折术后、膝关节周围截骨术后等各种膝关节疾病的晚期严重并发症之一。
膝关节软组织平衡技术:是指在膝关节置换过程中通过精准截骨、清理骨赘、松解粘连软组织及选择合适假体等一系列措施达到相等矩形的屈伸间隙及内外侧间隙紧张、松弛度适中等目的的技术。
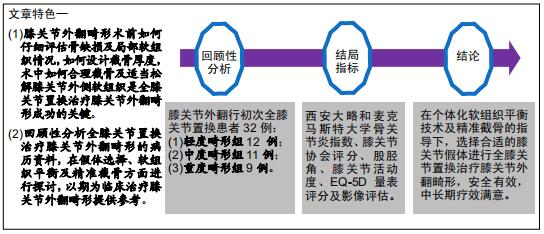
背景:膝关节外翻畸形的病例较少见而手术难度大,目前国内外的截骨及软组织平衡技术规范尚不统一。
目的:探讨人工全膝关节置换治疗膝关节外翻畸形的临床疗效。
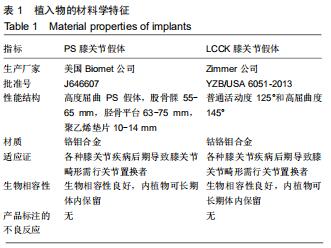
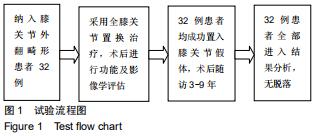
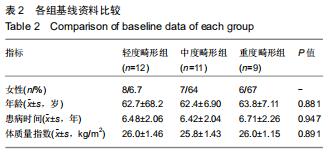
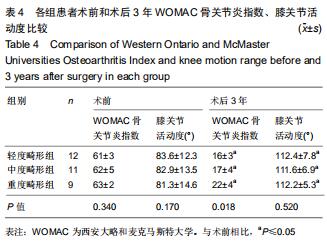
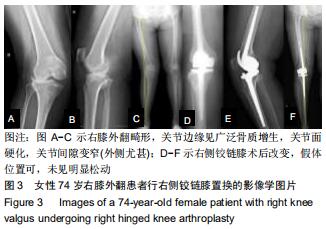
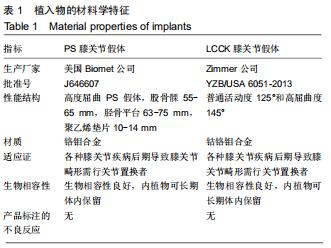
方法:回顾性分析2010年1月至2016年8月广州中医药大学第一附属医院收治的膝关节外翻畸形初次行人工全膝关节置换患者的病历资料,根据外翻程度进行分组,选择个体化软组织松解、精准截骨、合适假体及手术入路。评估患者术前、术后3年西安大略和麦克马斯特大学骨关节炎指数、膝关节协会评分、股胫角、膝关节活动度、EQ-5D量表评分,定期复查X射线片,观察膝关节有无松动和移位,并记录生存率及并发症情况。
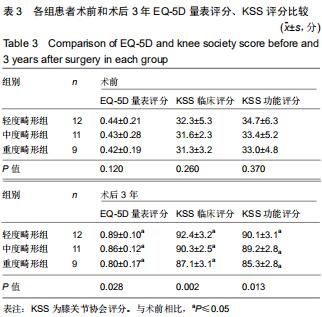
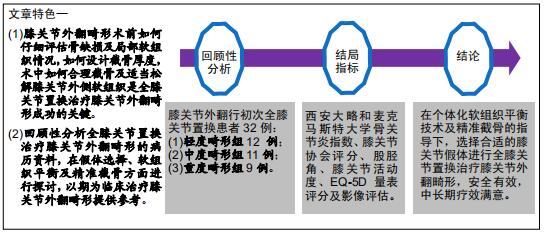
结果与结论:①共纳入32例患者(32膝),随访时间3-9年;②术后3年随访膝关节协会临床和功能评分均较术前明显增加,差异均有显著性意义(P < 0.05);术前不同畸形组别的膝关节协会临床和功能评分相比差异无显著性意义;术后3年不同畸形组别的膝关节协会临床和功能评分差异有显著性意义(P < 0.05),且轻度畸形组、中度畸形组评分要高于重度畸形组;③术后3年EQ-5D 量表评分与术前相比明显增加,差异有显著性意义(P < 0.05),术前不同畸形组别的EQ-5D量表评分相比差异无显著性意义,术后3年不同畸形组别的EQ-5D量表评分差异有显著性意义,且轻度畸形组、中度畸形组评分高于重度畸形组;④术后3年西安大略和麦克马斯特大学骨关节炎指数与术前相比明显降低,差异有显著性意义(P < 0.05);术前不同畸形组别的西安大略和麦克马斯特大学骨关节炎指数相比差异无显著性意义;术后不同畸形组别的西安大略和麦克马斯特大学骨关节炎指数差异有显著性意义(P < 0.05),且轻度畸形组、中度畸形组骨关节炎指数低于重度畸形组;⑤患者置换后膝关节活动度均明显增大,与术前相比差异有显著性意义(P < 0.05);术后不同畸形组别的膝关节活动度相比差异无显著性意义(P > 0.05);⑥随访期内膝关节假体固定良好,未出现松动及脱位,无明显深静脉血栓事件、假体感染等情况发生,假体生存率为100%;⑦提示在个体化软组织平衡技术及精准截骨的指导下,选择合适的膝关节假体进行全膝关节置换治疗膝关节外翻畸形安全有效,中长期疗效满意。
ORCID: 0000-0003-0023-4571(张朝鸣)中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号: