中国组织工程研究 ›› 2020, Vol. 24 ›› Issue (6): 962-967.doi: 10.3969/j.issn.2095-4344.2456
• 骨与关节循证医学 evidence-based medicine of the bone and joint • 上一篇 下一篇
全髋关节置换过程中使用保留股骨颈假体有效和安全性的系统评价
黄和涛1,潘建科2,杨伟毅2,曾令烽2,梁桂洪2,刘 军2
- 1广州中医药大学第二临床医学院,广东省广州市 510405;2广州中医药大学第二附属医院,广东省中医院,广东省广州市 510405
Systematic evaluation of the efficacy and safety of collum femoris preserving prosthesis in total hip arthroplasty
Huang Hetao1, Pan Jianke2, Yang Weiyi2, Zeng Lingfeng2, Liang Guihong2, Liu Jun2
- 1the Second Clinical Medical College of Guangzhou University of Chinese Medicine, Guangzhou 510405, Guangdong Province, China; 2the Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangdong Provincial Hospital of Chinese Medicine, Guangzhou 510405, Guangdong Province, China
摘要:
文题释义:
全髋关节置换:全髋关节由人工髋臼和人工股骨头组成,其假体类型和设计较多,主要是股骨头的直径和与骨固定的髋臼面的设计。全髋关节置换的并发症除有人工股骨头置换的并发症外,尚有人工髋臼的松动、脱位及负重区的超高分子聚乙烯面磨损后引发的局部反应。
保留股骨颈假体:意大利的Pipino教授通过对人工关节外科的深入研究,提出了“组织保护外科”的创新性理念,他认为在全髋关节置换术中应尽可能多的保留股骨近端健康骨组织以便用于固定髋关节股骨假体。他与德国Link公司合作,联合设计研发了保留股骨颈假体。
背景:保留股骨颈假体的全髋关节置换正在被越来越多的医生认可,但股骨颈假体保留与否对全髋关节置换疗效的影响暂时无法判断。
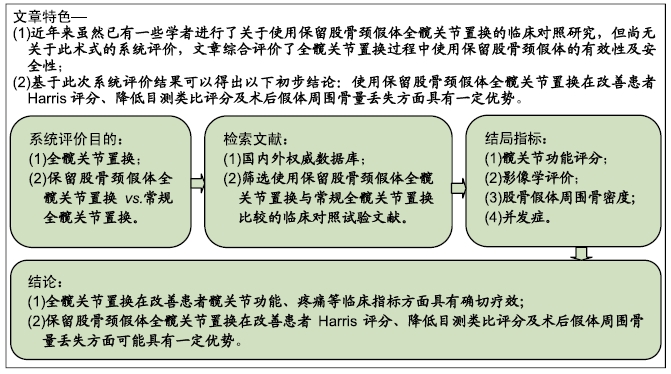
目的:系统评价全髋关节置换过程中使用保留股骨颈假体的有效性和安全性。
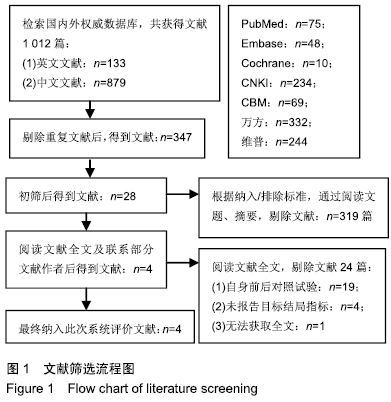
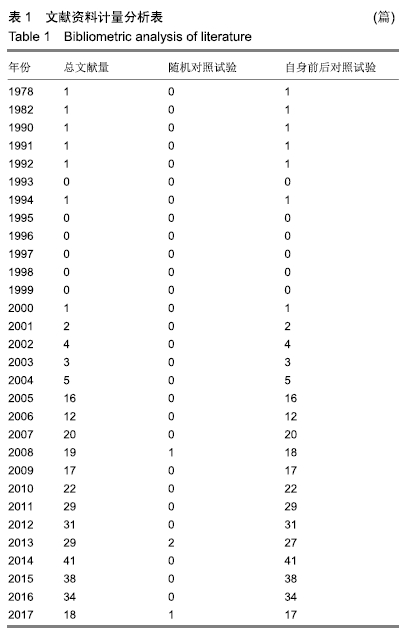
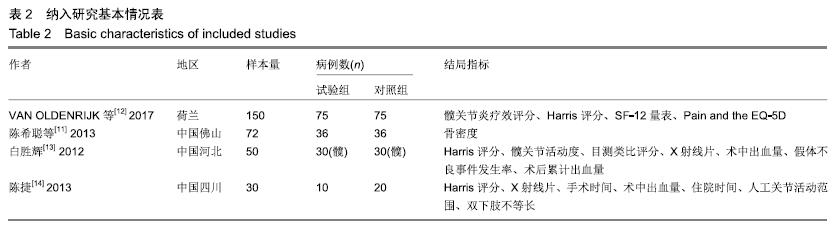
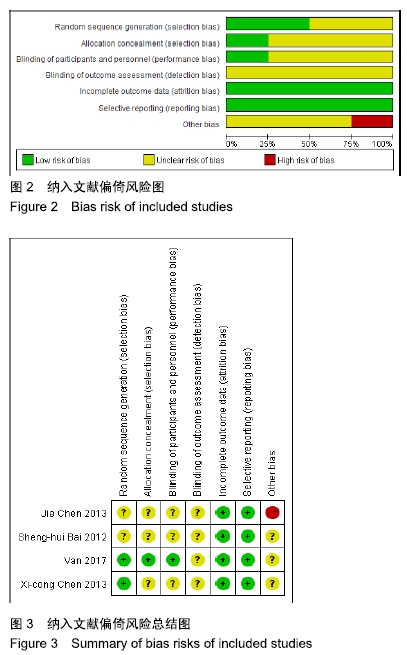
方法:系统检索中国生物医学文献数据库(CBM)、中国期刊全文数据库(中国知网/CNKI)、维普期刊数据库、万方资源数据库、PubMed、Embase、The Cochrane Library,检索截止时间为:2018-03-01。收集所有全髋关节置换过程中使用保留股骨颈假体的临床对照试验,并对其逐个进行方法学质量评价并采用RevMan 4.2软件进行系统评价。
结果与结论:①共纳入4篇研究,包括302例患者。由于纳入的研究及患者太少,且结局评价指标差异较大,不能进行Meta分析,只能进行描述性系统评价;②3个研究比较了2种手术方式在改善患者Harris评分方面的疗效差异,其中2个研究认为使用保留股骨颈假体全髋关节置换明显优于非保留股骨颈假体全髋关节置换 (P < 0.05),另1个研究则认为2种手术方式在改善Harris评分方面差异无显著性意义(P > 0.05);③2个研究比较了2种手术方式在改善患者关节活动度方面的疗效差异,1个研究结果显示使用保留股骨颈假体全髋关节置换明显优于非保留股骨颈假体全髋关节置换(P < 0.05),另1个研究结果则提示2种手术方式在改善患者关节活动度方面差异无显著性意义(P > 0.05);④1个研究结果显示使用保留股骨颈假体全髋关节置换组术后1年的假体周围骨量丢失明显少于非保留股骨颈假体全髋关节置换组(P < 0.05);⑤1个研究认为使用保留股骨颈假体全髋关节置换组在改善术后1年的目测类比评分方面优于非保留股骨颈假体全髋关节置换组(P < 0.05);⑥2个研究认为全髋关节置换术后1年无假体松动、下沉等不良假体事件发生;⑦2个研究比较了在手术时间、术中出血量方面的差异,结果显示2组患者在手术时间、术中出血量方面差异无显著性意义(P > 0.05);⑧1个研究认为使用保留股骨颈假体全髋关节置换组累计出血量高于非保留股骨颈假体全髋关节置换组(P < 0.05);⑨提示使用保留股骨颈假体全髋关节置换在改善患者Harris评分、降低目测类比评分及术后假体周围骨量丢失方面可能具有一定优势。尚需更多设计严格的研究以增加证据的强度。ORCID: 0000-0002-6197-1375(黄和涛)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号: