中国组织工程研究 ›› 2020, Vol. 24 ›› Issue (34): 5461-5466.doi: 10.3969/j.issn.2095-4344.2313
• 组织工程骨材料Tissue-engineered bone • 上一篇 下一篇
3D打印淫羊藿苷/脱钙骨基质修复兔股骨髁骨缺损
张虎雄1,李 微2,杨物鹏1,新苏雅拉图1
1鄂尔多斯市中心医院骨科,内蒙古自治区鄂尔多斯市 017000;2鄂尔多斯应用技术学院,内蒙古自治区鄂尔多斯市 017000
3D-printed icariin/decalcified bone matrix material promotes the repair of femoral condyle defects in rabbits
Zhang Huxiong1, Li Wei2, Yang Wupeng1, New Suyaratu1
1Department of Orthopedics, Ordos Central Hospital, Ordos 017000, Inner Mongolia Autonomous Region, China; 2Ordos Institute of Applied Technology, Ordos 017000, Inner Mongolia Autonomous Region, China
摘要:
文题释义:
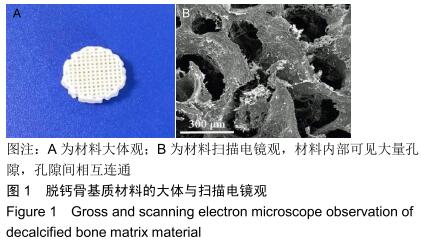
脱钙骨基质:主要由93%胶原、5%可溶性蛋白及2%残余矿化基质组成的商业化生物材料,包含不同浓度的骨形态发生蛋白、生长因子及转化生长因子,具备良好的骨传导与骨诱导能力,可以单独或联合其他材料广泛用于骨折、骨不连、骨肿瘤、骨融合、股骨头坏死等治疗中。
结构模型指数:是描述骨小梁组成结构中板层结构和杆状结构比例的参数。如果结构中骨小梁主要为板层结构,那么结构模型指数接近于0;如果结构中骨小梁主要为杆状结构,那么结构模型指数接近于3,该值越小骨小梁越成熟。
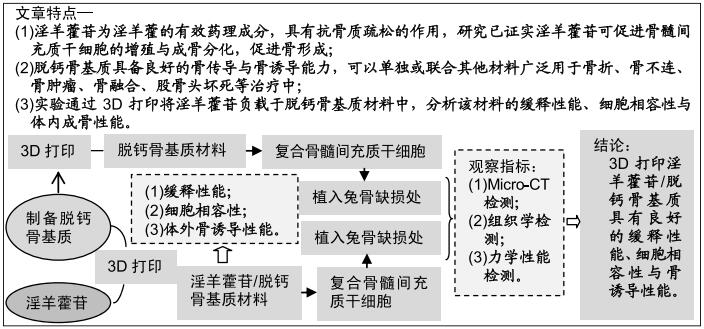
背景:淫羊藿苷可促进骨髓间充质干细胞的增殖与成骨分化,具有良好的促成骨性能。脱钙骨基质具备良好的骨传导与骨诱导能力,可以单独或联合其他材料广泛用于骨修复中。
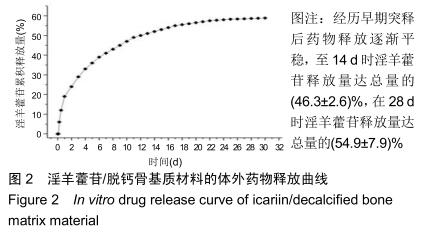
目的:观察3D打印淫羊藿苷/脱钙骨基质材料的缓释性能、细胞相容性与体内成骨性能。
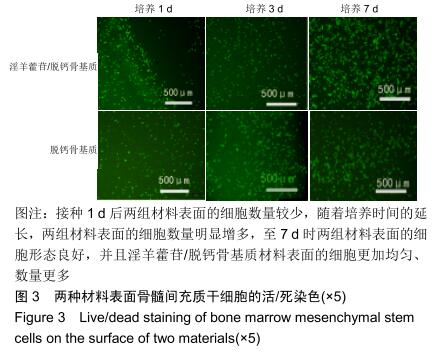
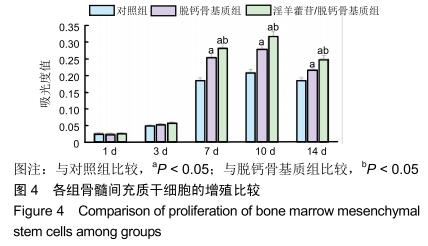
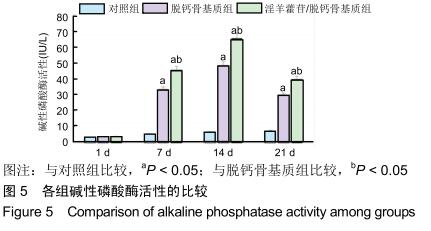
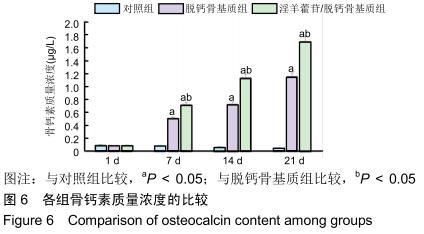
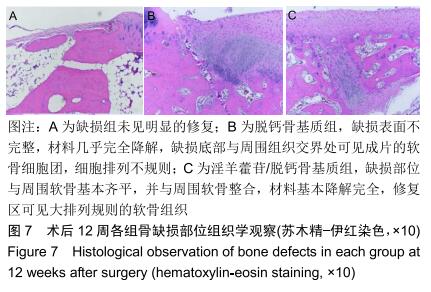
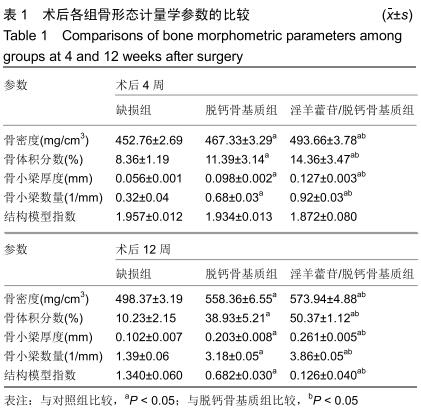
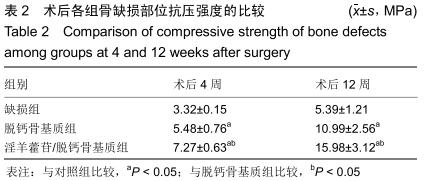
方法:利用3D打印技术制备淫羊藿苷/脱钙骨基质材料与脱钙骨基质材料,检测淫羊藿苷/脱钙骨基质材料的体外缓释性能。将骨髓间充质干细胞分别接种于两种材料表面,以单独培养的细胞为对照,于设定的时间点进行活/死染色、MTT、碱性磷酸酶活性与骨钙素含量检测。取新西兰大白兔30只,建立股骨髁骨缺损模型后分3组处理:对照组不植入任何材料,一组植入脱钙骨基质与同种异体兔骨髓间充质干细胞复合物,另一组植入淫羊藿苷/脱钙骨基质材料与同种异体兔骨髓间充质干细胞复合物,术后4,12周进行Micro-CT、组织学与力学性能检测。
结果与结论:①3D打印淫羊藿苷/脱钙骨基质材料具有缓释性能,在28 d时淫羊藿苷释放量达总量的(54.9±7.9)%;②活/死染色显示,接种1 d后两组材料表面的细胞数量较少,随着培养时间的延长,细胞数量明显增多,至7 d时细胞形态良好,并且淫羊藿苷/脱钙骨基质材料表面的细胞更加均匀、数量更多;③MTT检测显示,淫羊藿苷/脱钙骨基质组培养7,10,14 d的细胞增殖快于其余两组(P < 0.05);④淫羊藿苷/脱钙骨基质组培养7,10,14 d的碱性磷酸酶活性与骨钙素含量均高于其余两组(P < 0.05);⑤术后12周Micro-CT显示,植入材料两组均可见大量的骨小梁,其中淫羊藿苷/脱钙骨基质组骨小梁数量更多、骨小梁厚度增加、骨小梁分离度更小;⑥术后12周组织学显示,植入材料两组可见大量骨组织形成,其中淫羊藿苷/脱钙骨基质组新生骨量最多;⑦淫羊藿苷/脱钙骨基质组抗压强度高于其余两组(P < 0.05);⑧结果表明,3D打印淫羊藿苷/脱钙骨基质具有良好的缓释性能、细胞相容性与骨诱导性能。
ORCID: 0000-0002-5272-812X(张虎雄)
中国组织工程研究杂志出版内容重点:生物材料;骨生物材料; 口腔生物材料; 纳米材料; 缓释材料; 材料相容性;组织工程
中图分类号: