中国组织工程研究 ›› 2016, Vol. 20 ›› Issue (53): 7939-7945.doi: 10.3969/j.issn.2095-4344.2016.53.005
• 脊柱植入物 spinal implant • 上一篇 下一篇
腰椎单双侧钉棒系统置入内固定与非内固定修复腰椎间盘突出症的比较
王化瑾,张 健,盛伟斌
- 新疆医科大学第一附属医院脊柱外科,新疆维吾尔自治区乌鲁木齐市 830054
Lumbar unilateral and bilateral interbody fusion with internal fixation versus non-internal fixation for treating lumbar disc herniation
Wang Hua-jin, Zhang Jian, Sheng Wei-bin
- Department of Spinal Surgery, First Affiliated Hospital, Xinjiang Medical University, Urumqi 830054, Xinjiang Uygur Autonomous Region, China
摘要:
文章快速阅读:
.jpg)
文题释义:
腰椎间盘突出症:又称腰椎间盘纤维环破裂症,是指腰椎间盘发生退行性变,或外力作用导致椎间盘内外应力失衡,使椎间盘之纤维环破裂,髓核突出于纤维环之外,压迫脊髓(圆锥)、马尾、血管或神经根而产生的腰腿痛综合征。
椎间盘镜手术:对于椎间盘镜治疗腰椎间盘突出症,过去一些人认为其手术适应证受限制,但随着手术器械的发展及临床医生熟练程度的提高,其手术适应证已不再局限。在应用椎间盘镜过程中通过显示器可以清晰的看见术区解剖结构,减少不必要的损伤,术中可以保留更多的肌肉组织,减少损伤神经根的发生率,并且术中只咬除少量的黄韧带,对脊柱后柱结构损伤很小,最大限度的维持了脊柱的稳定性,术后可以有效的缓解患者症状。
摘要
背景:目前腰椎间盘突出症修复术式多种多样,主要通过摘除椎间盘,解除神经根压迫,以缓解患者症状,主要分为腰椎融合内固定术与非内固定术。
目的:比较腰椎融合内固定术与非内固定术修复腰椎间盘突出症的效果。
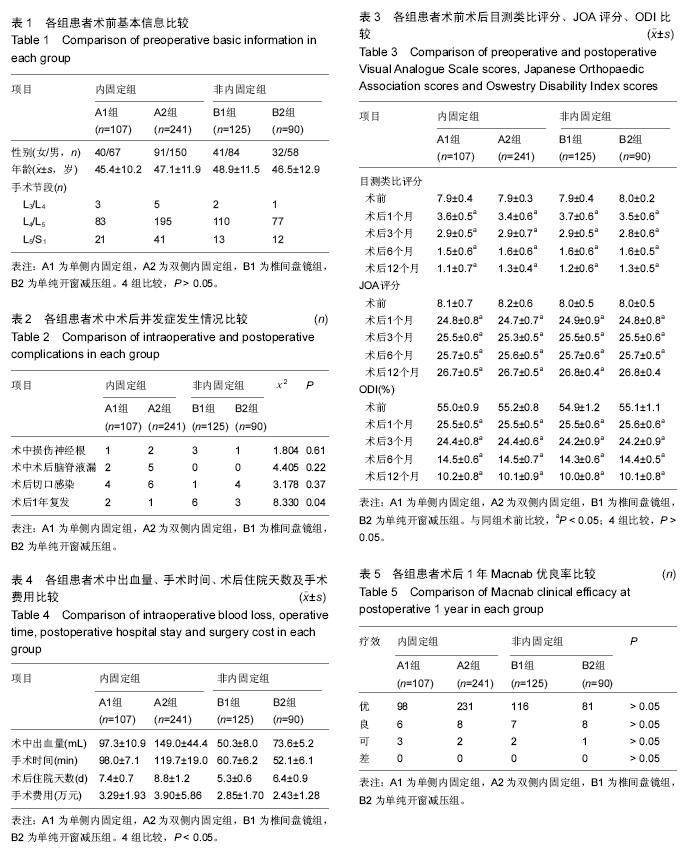
方法:回顾性分析563例腰椎间盘突出症手术治疗患者的临床资料,按照修复方式分组,A组为内固定组(348例),B组为非内固定组(215例),其中A组又分为单侧内固定组(A1组,107例)及双侧内固定组(A2组,241例),B组又分为椎间盘镜组(B1组,125例)及单纯开窗减压组(B2组,90例)。记录各组患者手术时间、术中出血量、术后住院时间、手术费用及手术相关并发症,比较4组术后1,3,6,12个月的目测类比评分、JOA评分及ODI,评估术后12个月Macnab优良率。
结果与结论:①各组术后目测类比评分、JOA评分、ODI均较术前显著改善(P < 0.05),术后随访1年,4组术后目测类比评分、JOA评分、ODI差异均无显著性意义(P > 0.05);术后患者Macnab优良率差异无显著性意义(P > 0.05);②患者术中神经根损伤、出现脑脊液漏及术后感染发生率差异均无显著性意义(P > 0.05),但患者术后复发率差异有显著性意义(P < 0.05),B1组术后复发率明显高于其他3组;③患者术中出血量、手术时间、术后住院时间及手术费用差异有显著性意义(P < 0.05),B1组术中出血量及术后住院天数明显低于其他3组,B2组手术时间及手术费用明显低于其他3组;④结果表明,目前腰椎间盘突出症的修复术式多种多样,无论内固定还是非内固定,在术后短期内均可获得较满意的修复效果,均可作为修复腰椎间盘突出症的有效术式。
中图分类号:

.jpg)
.jpg)