Knee arthritis arthrogenous muscle weakness and muscle function decrease
Joint injury/pain-induced muscle inhibition and secondary muscle atrophy-induced muscle weakness are called arthrogenous muscle weakness[4]. Knee joint osteoarthritis-induced pain could cause arthrogenous muscle weakness. On the contrary, abnormal function of relevant muscles also decreased joint stability, and further accelerated joint injury. Muscle function disturbance secondary to osteoarthritis is a major factor for progressive aggravation of osteoarthritis[5].
Slemenda
et al [6] found that muscle weakness already appeared when knee joint pain or muscle atrophy did not appear, and assumed that this kind of muscle weakness was probably induced by abnormal function of muscles. They also supported that muscle weakness was possibly a risk factor for the occurrence and development of knee joint osteoarthritis.Pang
et al [7] confirmed that muscle strength obviously reduced in the lower limbs of affected side, which was mainly induced by the reduction in muscle function.
Shi et al [8-9] compared the muscle contraction and coordination among muscles of medial vastus muscle, rectus femoris muscle and vastus lateralis between knee osteoarthritis patients and normal persons using surface electromyogram and isokinetic muscle strength test, and verified that contraction speed of medial vastus muscle, rectus femoris muscle and vastus lateralis was slow down, and contraction strength was decreased in knee osteoarthritis patients. The coordination of quadriceps femoris diminished on the affected side. Muscle contraction force decreased and muscle contraction was not coordinated on the affected side. Muscle strength balance was disordered, so muscle functions were decreased.
Yu et al [10] tested surface electromyogram signals during isometric muscular contraction and squatting in 26 patients with unilateral knee osteoarthritis using Noraxon Myosystem
1 200 electromyographic system, and demonstrated that muscle function decrease and muscle strength unbalance possibly existed under different motor conditions on the affected side.
Previous studies reported that muscle dysfunction was detected on the affected side in knee osteoarthritis patients[11-14]. Therefore, muscle weakness is a key element involved in pathological process of knee osteoarthritis.
The Hospital for Special Surgery knee score after total knee replacement
The main aim of knee joint replacement was to remove severe degenerative articular surface and osteophyte, to correct genu varum and genu valgum, to lessen patient’s pain, to improve patient’s walking ability, and to elevate quality of life of severe degenerative arthritis patients. In this study, the mean score of the replacement side was 91.44, and the excellent and good rate of the surgery was 100%. Pain and joint function were significantly improved after knee replacement. Mean score of the non-replacement side was 54.52. It is clear that knee replacement for knee osteoarthritis showed noticeable clinical therapeutic effects, which was consistent with a previous study[15].
Myoelectric activity of the lower limb muscles after knee replacement
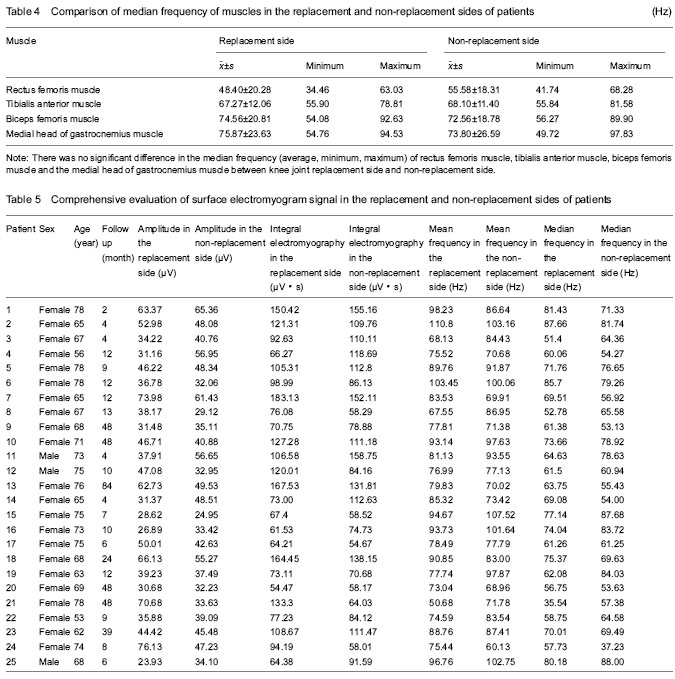
Surface electromyogram signal refers to one-dimensional time series signal of bioelectric change during neuromuscular system activity after guiding, amplifying, revealing and recording on the surface of skin. The obtained amplitude, integral electromyography, mean frequency, and median frequency (mean, minimum and maximum) reflected muscular activity, evaluated muscle fatigue, and indirectly assessed the strength of work muscle, and are perfect indexes for the evaluation of muscle function in the clinic[16].
Some scholars believed that muscle strength of knee joint was strongly associated with pain and activity of the knee joint. After knee replacement, pain was relieved, walking function increased, and the function of muscles surrounding the knee joint also increased[17]. Other scholars also thought that after total knee replacement, knee joint’s pain was removed and function was improved, but muscular function was recovered in only a small part of patients[18]. A previous study verified that during knee replacement[19], stripping and implant placement induced quadriceps femoris atrophy and decreased muscular strength. Alterations in lower limb alignment and the existence of scar tissue after surgery affected the force along muscle or tendon. Thus, it is hard to restore the normal level for quadriceps femoris after replacement.
Wang et al [20] observed the effects of massage and rehabilitation on surface electromyography in rheumatoid arthritis patients in early stage after total knee replacement, and results suggested that after 4 weeks of massage, mean frequency and integral electromyography of rectus femoris and vastus medialis were significantly increased in the massage group (P < 0.01). Bai et al [21] observed time-distance parameters, kinematics parameters, mechanics parameters and dynamic myoelectric parameters in healthy persons and patients with spinal column, hip, knee and ankle joint diseases. Dynamic myoelectric parameters revealed that surface electromyogram signal of left vastus lateralis was obviously weaker than that on the right side at 1 year after left total knee replacement.
Results from the present study displayed that significant differences in amplitude, integral electromyography, mean frequency, and median frequency (mean, minimum and maximum) of rectus femoris muscle, tibialis anterior muscle, and biceps femoris muscle were not detected between knee joint replacement side and non-replacement side (P > 0.05). There were also no significant differences in mean frequency and median frequency (mean, minimum and maximum) in the medial head of gastrocnemius muscle between knee joint replacement side and non-replacement side (P > 0.05). These results suggested that the arthrogenous muscle weakness and muscle function decrease did not improve after replacement in knee osteoarthritis patients. The function of muscles surrounding the knee joint did not recover after replacement, which was consistent with previous studies[18-19]. During knee replacement, the incision was opened under anesthesia. Osteophyte, partial fat pad and meniscus were scavenged. Using an instrument for ostectomy, after soft tissue release, the prosthesis was placed, and the incision was closed. The damaged articular surface was replaced. Inflammatory substance was removed, and pain was lessened. Big muscles were not treated during knee replacement. The requirements were relatively low in patients, and their concept on muscular function exercises was weak. In addition, some patients were older, had long disease course, and abnormal muscle tissues. Therefore, the function of muscles surrounding knee joint is hard to be recovered.
Results from this study showed that amplitude and integral electromyography (average, minimum, maximum) in the medial head of gastrocnemius muscle were higher in the replacement side than those in non-replacement side (P < 0.05). There were differences in dominant limbs in normal persons, and significant differences in amplitude and integral electromyography were detectable between left and right medial head of gastrocnemius muscle[22]. Taken together, there were significant differences in amplitude and integral electromyography in the medial head of gastrocnemius muscle between the replacement side and non-replacement side, which hardly indicated the increased function in muscles surrounding knee joint after knee replacement.
In conclusion, after knee replacement, pain, malformation, and walking ability were obviously improved on the replacement side. However, muscles (rectus femoris muscle, tibialis anterior muscle, biceps femoris muscle and the medial head of gastrocnemius muscle) surrounding knee joint did not restore to the normal activity level. Unrestored muscular function is probably the reason for knee osteoarthritis relapse and prosthesis re-replacement at 10-15 years after knee replacement. Even symptoms were significantly improved after total knee replacement, to elevate therapeutic effect, especially the long-period effects, we cannot neglect the muscular functions. With gradually improved technique of prosthesis and replacement, muscular rehabilitation technology also gradually elevated. The perfect combination of knee replacement and muscular rehabilitation can reach a long-period therapeutic effect.