中国组织工程研究 ›› 2018, Vol. 22 ›› Issue (23): 3751-3758.doi: 10.3969/j.issn.2095-4344.0286
• 骨与关节循证医学 evidence-based medicine of the bone and joint • 上一篇 下一篇
初次全膝关节置换后放置引流管疗效和安全关系的Meta分析
唐 健,王仁崇,汤中飞,李百川
- 柳州市工人医院西院运动医学及肩肘外科,广西壮族自治区柳州市 545001
Efficacy and safety of drainage placement after primary total knee arthroplasty: a meta-analysis
Tang Jian, Wang Ren-chong, Tang Zhong-fei, Li Bai-chuan
- Department of Shoulder and Elbow Surgery, West Branch of Liuzhou Worker’s Hospital, Liuzhou 545001, Guangxi Zhuang Autonomous Region, China
摘要:
文章快速阅读:
.jpg)
文题释义:
深静脉血栓:是指血液非正常地在深静脉内凝结,属于下肢静脉回流障碍性疾病。血栓形成大都发生于制动状态(尤其是骨科大手术)。致病因素有血流缓慢、静脉壁损伤和高凝状态三大因素。血栓形成后,除少数能自行消融或局限于发生部位外,大部分会扩散至整个肢体的深静脉主干,若不能及时诊断和处理,多数会演变为血栓形成后遗症,长时间影响患者的生活质量;还有一些患者可能并发肺栓塞,造成极为严重的后果。
引流:在外科中通常将瘀积在关节腔内、体腔内器官或组织的液体引离原处和排出体外的过程称为引流。骨科大手术后临床医师通常会放置引流装置,而有相关研究表明放置引流与否在置换后血红蛋白下降程度和功能恢复方面无明显差异,而作为切口与引流装置接触处为细菌提供了可能的入侵门户,引流导致伤口内血肿填塞作用消失,伤口内压力下降导致伤口出血量增加,但有学者认为外科手术后放置引流可减少血肿形成及减轻切口压力。
摘要
背景:全膝关节置换在治疗膝关节终末期疾病时可以有效缓解患者的疼痛、重建膝关节功能,目前已在临床上广泛应用,但对于全膝关节置换后是否放置引流管目前仍存在一定的争议。
目的:通过Meta分析评价是否放置引流对初次全膝关节置换的临床疗效影响及并发症。
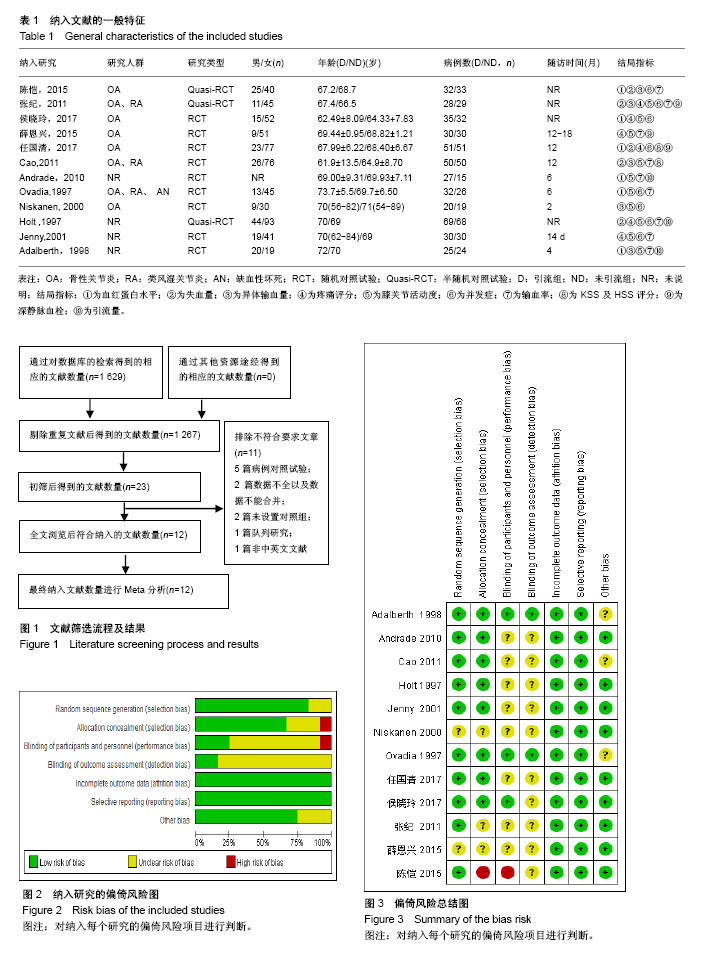
方法:通过计算机检索PubMed,Embase,Cochrane图书馆,万方数据库及中国知网5个数据库,检索与初次单侧全膝关节置换后是否放置引流装置的所有临床随机对照试验以及半随机对照试验。收集纳入相关研究文献的数据,对能进行合并分析的研究采用Revman 5.3软件进行Meta分析,结局指标包括置换后血红蛋白、输血率、失血量、异体输血量、目测类比疼痛评分、膝关节活动度、膝关节功能评分、并发症以及深静脉血栓发生率。
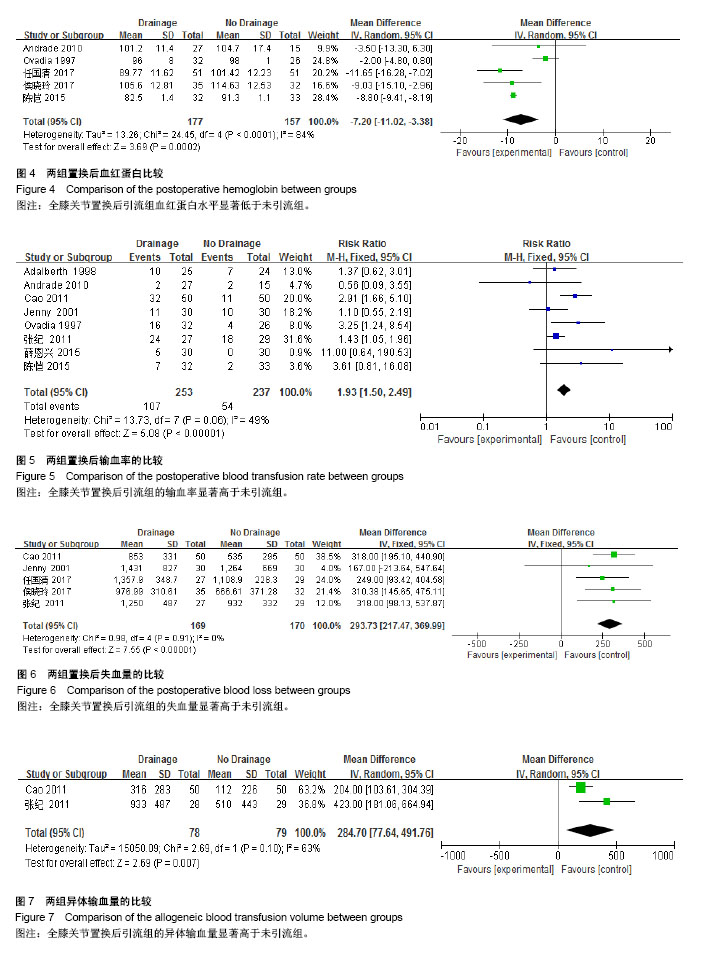
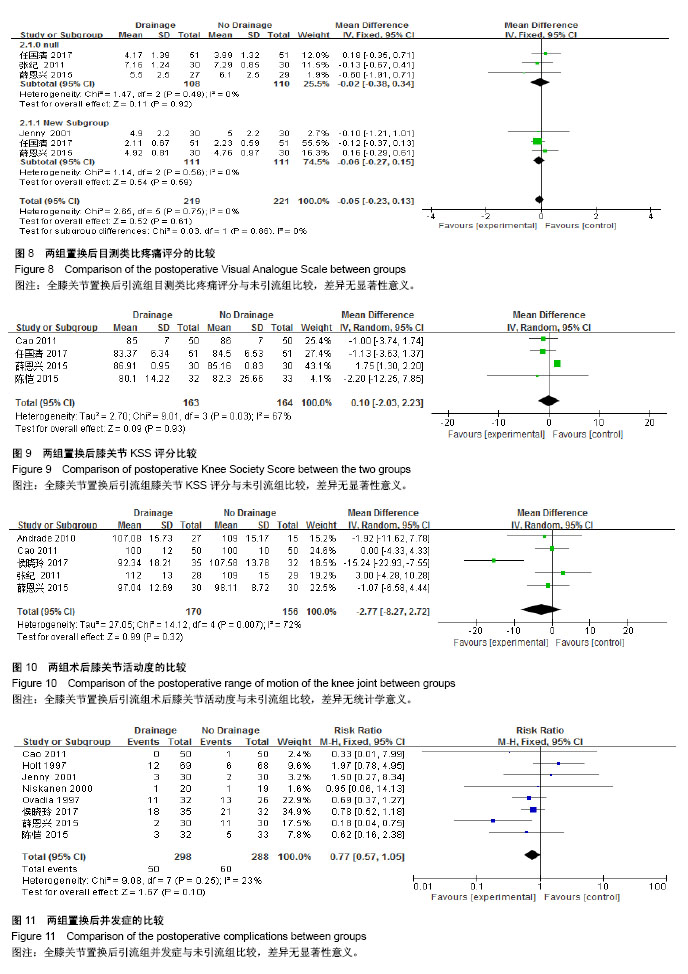
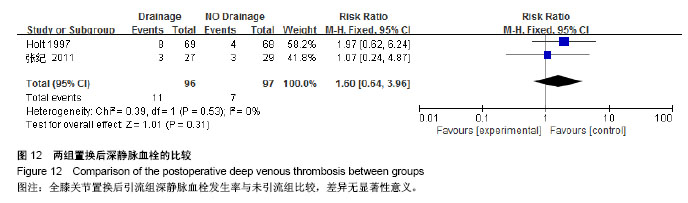
结果与结论:①共纳入12篇文献,其中包括9篇随机对照试验,3篇半随机对照试验,总共836例患者。其中引流组为429例,未引流组为407例;②Meta分析结果显示:初次单侧全膝关节置换后,与未引流组比较,引流组在置换后血红蛋白[MD=-7.20,95%CI(-11.02,-3.38),P=0.000 2],输血率[RR=1.93,95%CI(1.50,2.49),P < 0.000 01],失血量[MD=293.73,95%CI(217.47,369.99),P < 0.000 01],异体输血量[MD=284.70,95%CI(77.64,491.76),P=0.007]方面差异具有显著性意义。但是在置换后第1天目测类比疼痛评分[MD=-0.02,95%CI(-0.38,0.34),P=0.92],置换后第7天目测类比疼痛评分[MD=-0.06,95%CI(-0.27,0.15),P=0.86],膝关节KSS评分[MD=0.10,95%CI(-2.03,2.23),P=0.93],膝关节活动度[MD=-2.77,95%CI(-8.27,2.72),P=0.32],并发症[RR=0.77,95%CI(0.57,1.05),P=0.10],深静脉血栓[RR=1.60,95%CI(0.64,3.96),P=0.31]方面,差异无显著性意义;③结果提示,初次全膝关节置换后放置引流管会增加置换后失血、输血率以及输血量,但是不会提高膝关节的功能,减轻置换后疼痛以及并发症,因此全膝关节置换后尽量减少放置引流装置。
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
ORCID: 0000-0002-6328-1773(唐健)
中图分类号:
.jpg)