中国组织工程研究 ›› 2018, Vol. 22 ›› Issue (11): 1743-1748.doi: 10.3969/j.issn.2095-4344.0173
• 骨与关节图像与影像 bone and joint imaging • 上一篇 下一篇
腰椎椎弓根CT影像学参数的测量与临床意义
管喆恒1,杨惠林1,罗宗平2,崔旭东2,潘晓宇3,严沫琦1,王一帆2,陆霁航2
- 1苏州大学第一附属医院,江苏省苏州市 215006;2苏州大学南校区骨科研究所,江苏省苏州市 215000;3北京大学第三医院,北京市 100191
Measurement and clinical significance of lumbar pedicle CT imaging parameters
Guan Zhe-heng1, Yang Hui-lin1, Luo Zong-ping2, Cui Xu-dong2, Pan Xiao-yu3, Yan Mo-qi1, Wang Yi-fan2, Lu Ji-hang2
- 1First Affiliated Hospital, Soochow University, Suzhou 215006, Jiangsu Province, China; 2Orthopedic Institute, South Campus of Soochow University, Suzhou 215000, Jiangsu Province, China; 3Third Hospital, Peking University, Beijing 100191, China
摘要:
文章快速阅读:
.jpg)
文题释义:
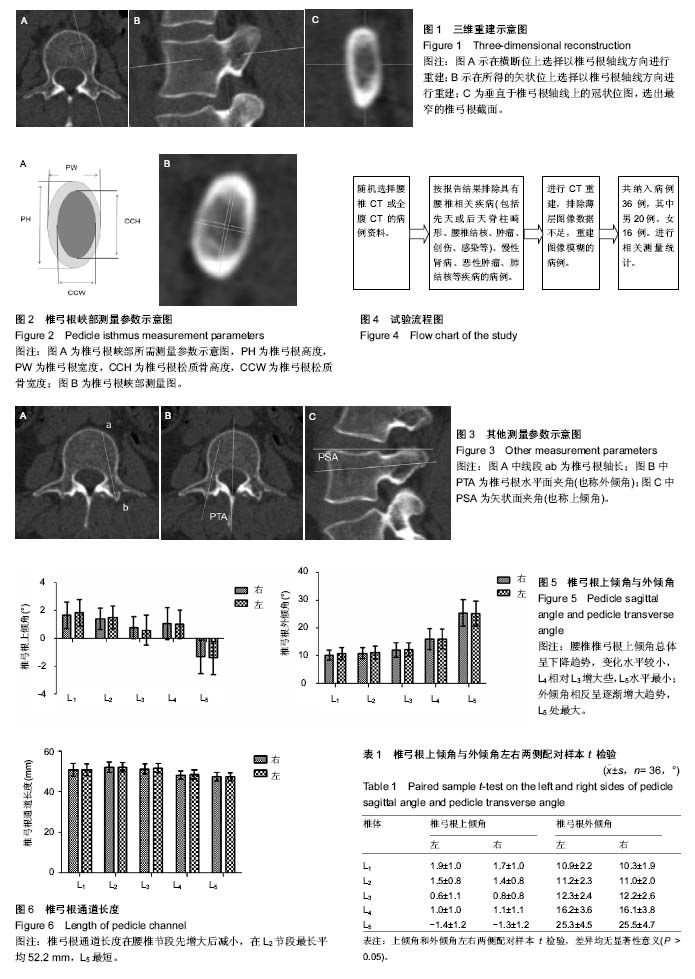
测量椎弓根解剖学形态的方法:目前测量椎弓根解剖学形态的方法主要有:①用游标卡尺直接在尸体标本进行测量;②运用X射线进行尸体或活体测量;③对尸体或活体CT平扫测量;④运用螺旋CT技术对尸体或活体进行三维重建及测量。由于椎弓根结构的特殊性,前3种方法均无法很好的了解及展现其内部形态,而多排螺旋CT重建技术在研究椎弓根通道内部结构形态方面具有很大优势。这项技术可从任意平面对对象进行重建,能更清晰准确地测量。
CT重建:通常根据CT平扫获得的物体数据来重新建立图像,骨科常用的有三维重建和表面重建。而多平面重建是从原始的横轴位图像经后处理获得人体组织器官任意的冠状、矢状、横轴和斜面的二维图像处理方法,与MR图像十分相近,显示全身各个系统器官的形态学改变,尤其在判断颅底、颈部、肺门、纵隔、腹部、盆腔及大血管等解剖结构和器处理官的病变性质、侵及范围和毗邻关系有着明显优势。
摘要
背景:尽管随着技术的发展,越来越多精确、个性化的检测和辅助工具应用于骨科领域,但是目前术前CT依然是众多骨科医师的一线检查手段。因此掌握腰椎椎弓根的CT影像学表现是脊柱外科医生的基础,也是脊柱置钉手术的基石。
目的:通过CT影像技术,测量国人腰椎椎弓根影像学参数,了解其内部结构规律作为螺钉选择的依据,以提高置钉手术的安全性与准确性。
方法:随机选择36例于苏州大学第一附属医院行腰椎及腹腔CT检查但无腰椎相关疾病的病例,其中男20例,女16例,年龄(43.3±12.3)岁。应用PACS系统进行腰椎重建,测量相关影像学参数。
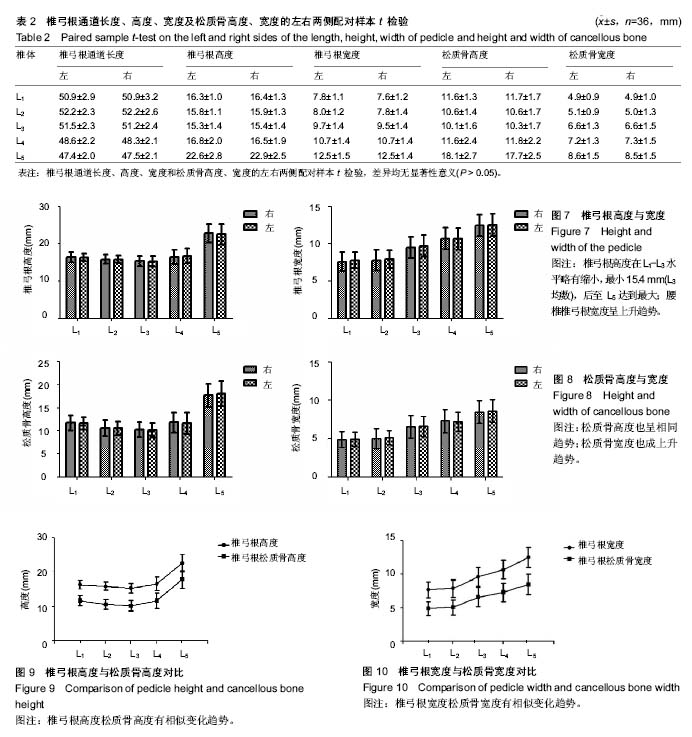
结果与结论:①病例自身左右两侧椎弓根各参数进行配对样本t检验,差异均无显著性意义(P > 0.05);②腰椎椎弓根上倾角总体呈下降趋势,变化水平较小,L4相对L3增大些,L5水平最小,平均为-1.3°;外倾角相反呈逐渐增大趋势,L5处最大,均数为25.4°;③椎弓根通道长度在腰椎节段先增大后减小,在L2节段最长平均52.2 mm,L5最短,平均47.4 mm;④椎弓根高度在L1-L3水平略有缩小,最小15.4 mm(L3均数),后至L5达到最大,可达22.7 mm(L5均数);松质骨高度也呈相同趋势,最小L3为10.2 mm,最大L5为17.9 mm;⑤腰椎椎弓根宽度呈上升趋势,L1最小为7.7 mm,L5最大为12.5 mm;松质骨宽度也成相似上升趋势,最窄L1平均为4.9 mm,最大L5平均为8.5 mm;⑥总体上看,上腰椎椎弓根通道细长,而下腰椎稍粗短;⑦综上,通过对椎弓根形态参数的测量,其相关参数可以成为选择合适螺钉的依据。同时,腰椎各节段椎弓根形态具有一定差异也存在一定规律,准确把握其结构与影像特点是椎弓根螺钉置钉手术的基础。而术前影像资料的收集评估,结合患者一般情况,制定个性化的置钉方案,在提高置钉的安全性和准确性方面有所帮助。
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
ORCID: 0000-0002-0170-2333(管喆恒)
中图分类号:
.jpg)