[1] LONG Y, YI W, YANG D. Advances in Vertebral Augmentation Systems for Osteoporotic Vertebral Compression Fractures. Pain Res Manag. 2020;2020: 3947368.
[2] 马晓勇,高飞,万英辉,等.绝经后骨质疏松性骨折治疗与再骨折的关系研究[J].河北医药,2020,42(2):261-264.
[3] 曹建康.骨质疏松性椎体压缩骨折患者再发椎体压缩骨折的危险因素分析[D].济南:山东大学,2019.
[4] 邱贵兴,裴福兴,胡侦明,等.中国骨质疏松性骨折诊疗指南——骨质疏松性骨折诊断及治疗原则[J].黑龙江科学,2018,9(2):85-88+95.
[5] 马云萍,王雍立,顾学群.绝经后老年OVCF患者单侧穿刺入路PKP后应用骨化三醇、钙剂及降钙素三联疗效分析[J]. 中国地方病防治杂志,2022,37(6): 524-527.
[6] 邓强,乔小万,李中锋,等.骨质疏松性椎体压缩骨折椎体成形术后非手术椎体再骨折危险因素探讨[J].中国骨质疏松杂志,2021,27(4):613-617+624.
[7] QIN K, TIAN H, ZHANG K, et al. Risk Factors for Hidden Blood Loss Associated with Vertebroplasty or Kyphoplasty for Osteoporotic Vertebral Compression Fracture: A Systematic Review and Meta-Analysis. World Neurosurg. 2023;175:47-56.
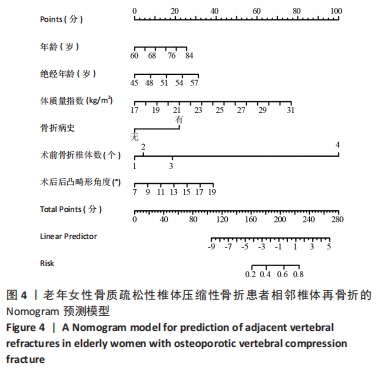
[8] LI Q, LONG X, WANG Y, et al. Development and validation of a nomogram for predicting the probability of new vertebral compression fractures after vertebral augmentation of osteoporotic vertebral compression fractures. BMC Musculoskelet Disord. 2021;22(1):957.
[9] PARK JS, PARK YS. Survival analysis and risk factors of new vertebral fracture after vertebroplasty for osteoporotic vertebral compression fracture. Spine J. 2021;21(8):1355-1361.
[10] HU H, CAO KX, HUANG P, et al. Risk factors of adjacent vertebral refracture after percutaneous vertebroplasty for osteoporotic vertebral compression fractures in super-old patients. Zhongguo Gu Shang. 2022;35(8):710-714.
[11] 张智海,刘忠厚,李娜,等.中国人骨质疏松症诊断标准专家共识(第三稿·2014版)[J].中国骨质疏松杂志,2014,20(9):1007-1010.
[12] 张保健,周红星.骨水泥弥散对经皮椎体成形术治疗骨质疏松性椎体压缩骨折疗效的影响[J].临床骨科杂志,2022,25(1):20-24.
[13] 段克友,刘翔宇,熊风,等.绝经后骨质疏松症患者发生骨质疏松性椎体压缩骨折危险因素分析[J].山东医药,2021,61(24):34-38.
[14] 邵旭辉,王冠军,王登基.胸腰椎压缩性骨折患者经皮椎体成形术后发生邻近椎体再骨折的影响因素[J]. 河南医学研究,2023,32(5):877-880.
[15] 李坚,张金喜,张海明,等.PKP与PVP在骨质疏松性椎体压缩骨折术后疼痛及椎体高度恢复的比较[J]. 浙江创伤外科,2022,27(6):1077-1079.
[16] 欧阳少明,饶放萍,刘辉,等.绝经后妇女骨质疏松性压缩骨折PVP、PKP治疗效果及优劣势比较[J].中国老年学杂志,2020,40(1):99-102.
[17] YANG D, TAN J, LONG Y, et al. Sequential treatment of teriparatide and alendronate versus alendronate alone for elevation of bone mineral density and prevention of refracture after percutaneous vertebroplasty in osteoporosis: a prospective study. Aging Clin Exp Res. 2023;35(3):531-539.
[18] YANG Z, XING D, DONG Z, et al. Epidemiological Investigation of 387 Individuals Over 65 Years Old With Osteoporotic Fractures. Altern Ther Health Med. 2023;29(3):207-211.
[19] 王徐龙,魏建仝,要鹏.老年骨质疏松性椎体压缩性骨折PVP术后再骨折风险的列线图预测模型构建[J].中国老年学杂志,2023,43(8):1836-1839.
[20] JACKSON A, WASFIE T, BROCK C, et al. Fragility Vertebral Compression Fractures in Postmenopausal Women: The Role of a Fracture Liaison Service Program. Am Surg. 2020;86(12):1636-1639.
[21] CHO MJ, MOON SH, LEE JH, et al. Association between Osteoporotic Vertebral Compression Fractures and Age, Bone Mineral Density, and European Quality of Life-5 Dimensions in Korean Postmenopausal Women: A Nationwide Cross-sectional Observational Study. Clin Orthop Surg. 2021;13(2):207-215.
[22] 于利平,白勇涛,罗笑婵,等.北京社区绝经后女性骨质疏松性骨折相关危险因素和防治现况[J].中华骨质疏松和骨矿盐疾病杂志,2020,13(2):110-115.
[23] 张保良,陈允震.骨质疏松性椎体压缩骨折住院患者的人口学特征及临床特征分析[J].中华骨科杂志,2019,39(24):1523-1535.
[24] FISTAROL M, REZENDE CR, FIGUEIREDO CAMPOS AL, et al. Time since menopause, but not age, is associated with increased risk of osteoporosis. Climacteric. 2019;22(5):523-526.
[25] ZHANG J, ZHANG T, XU X, et al. Zoledronic acid combined with percutaneous kyphoplasty in the treatment of osteoporotic compression fracture in a single T12 or L1 vertebral body in postmenopausal women. Osteoporos Int. 2019; 30(7):1475-1480.
[26] CHENG Y, CHENG X, WU H. Risk factors of new vertebral compression fracture after percutaneous vertebroplasty or percutaneous kyphoplasty. Front Endocrinol (Lausanne). 2022;13:964578.
[27] LEE BG, CHOI JH, KIM DY, et al. Risk factors for newly developed osteoporotic vertebral compression fractures following treatment for osteoporotic vertebral compression fractures. Spine J. 2019;19(2):301-305.
[28] 马一鸣,王子豪,蔡大钊,等.椎体后凸成形治疗骨质疏松性椎体压缩骨折后新发骨折危险因素预测模型的建立[J].中国组织工程研究,2023,27(23): 3700-3706.
[29] 李杰,王祥善,张华.骨质疏松性椎体压缩性骨折经皮椎体后凸成形术后再骨折的危险因素分析[J].河南外科学杂志,2023,29(2):144-146.
[30] MAO W, DONG F, HUANG G, et al. Risk factors for secondary fractures to percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a systematic review. J Orthop Surg Res. 2021;16(1):644.
[31] LI W, WANG H, DONG S, et al. Establishment and validation of a nomogram and web calculator for the risk of new vertebral compression fractures and cement leakage after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. Eur Spine J. 2022;31(5):1108-1121.
[32] ZHAO C, LIU X, WANG Y, et al. The effects of biomechanical factors on adjacent vertebral compression fractures after percutaneous kyphoplasty: a propensity score matching analysis. Osteoporos Int. 2022;33(8):1795-1806.
[33] LI YX, GUO DQ, ZHANG SC, et al. Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP). Int Orthop. 2018;42(9):2131-2139.
[34] OKUWAKI S, FUNAYAMA T, IKUMI A, et al. Risk factors affecting vertebral collapse and kyphotic progression in postmenopausal osteoporotic vertebral fractures. J Bone Miner Metab. 2022;40(2):301-307.
|