[1] JEON I, KIM SW, YU D. Paraspinal muscle fatty degeneration as a predictor of progressive vertebral collapse in osteoporotic vertebral compression fractures. Spine J. 2022;22(2):313-320.
[2] PATEL D, LIU J, EBRAHEIM NA. Managements of osteoporotic vertebral compression fractures: A narrative review. World J Orthop. 2022;13(6): 564-573.
[3] MAO W, DONG F, HUANG G, et al. Risk factors for secondary fractures to percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a systematic review. J Orthop Surg Res. 2021;16(1):644.
[4] ZHANG ZL, YANG JS, HAO DJ, et al. Risk Factors for New Vertebral Fracture After Percutaneous Vertebroplasty for Osteoporotic Vertebral Compression Fractures. Clin Interv Aging. 2021;16:1193-1200.
[5] MA CH, YANG HL, HUANG YT, et al. Effects of percutaneous vertebroplasty on respiratory parameters in patients with osteoporotic vertebral compression fractures. Ann Med. 2022;54(1):1320-1327.
[6] CHENG J, JU S, ZHANG Z. Osteoporotic vertebral compression fractures caused by Cushing’s syndrome in young women: case report and literature review. BMC Musculoskelet Disord. 2023;24(1):167.
[7] LIU D, XU J, WANG Q, et al. Timing of Percutaneous Balloon Kyphoplasty for Osteoporotic Vertebral Compression Fractures. Pain Physician. 2023;26(3):231-243.
[8] ZHAO Y, ZHANG T, TANG P. Diagnostic value of SPECT/CT bone imaging in fresh osteoporotic vertebral compression fractures. Hell J Nucl Med. 2022;25(2):138-142.
[9] LIN S, CAI X, CHENG Q, et al. Association between bone turnover markers, BMD and height loss of cemented vertebrae after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Orthop Surg Res. 2022;17(1):202.
[10] COSMAN F, DE BEUR SJ, LEBOFF MS, et al. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014; 25(10):2359-2381.
[11] PRATHER H, WATSON JO, GILULA LA. Nonoperative management of osteoporotic vertebral compression fractures. Injury. 2007;38 Suppl 3: S40-48.
[12] KUTSAL FY, ERGIN ERGANI GO. Vertebral compression fractures: Still an unpredictable aspect of osteoporosis. Turk J Med Sci. 2021;51(2): 393-399.
[13] HU ZA, FAN SW. Current situation analysis of diagnosis and treatment for osteoporotic vertebral compression fractures. Zhongguo Gu Shang. 2022;35(5):405-408.
[14] BIAN F, BIAN G, AN Y, et al. Establishment and Validation of a Nomogram for the Risk of New Vertebral Compression Fractures After Percutaneous Vertebroplasty in Patients With Osteoporotic Vertebral Compression Fractures: A Retrospective Study. Geriatr Orthop Surg Rehabil. 2022;13:21514593221098620.
[15] FAN N, WANG T, WANG A, et al. A predictive nomogram for intradiscal cement leakage in percutaneous kyphoplasty for osteoporotic vertebral compression fractures combined with intravertebral cleft. Front Surg. 2022;9:1005220.
[16] DAHER M, KREICHATI G, KHARRAT K, et al. Vertebroplasty versus Kyphoplasty in the Treatment of Osteoporotic Vertebral Compression Fractures: A Meta-Analysis. World Neurosurg. 2023;171:65-71.
[17] MILLS ES, TON AT, BOUZ G, et al. Acute Operative Management of Osteoporotic Vertebral Compression Fractures Is Associated with Decreased Morbidity. Asian Spine J. 2022;16(5):634-642.
[18] LIU H, WANG W, HUANG Y, et al. Influence of Different Surgical Timing after Percutaneous Kyphoplasty for Osteoporotic Vertebral Compression Fractures: A Retrospective Study. Int J Clin Pract. 2022;2022:7500716.
[19] PATEL N, JACOBS D, JOHN J, et al. Balloon Kyphoplasty vs Vertebroplasty: A Systematic Review of Height Restoration in Osteoporotic Vertebral Compression Fractures. J Pain Res. 2022;15:1233-1245.
[20] JIANG J, ZHANG J, BAO G, et al. Percutaneous vertebral-disc plasty for thoracolumbar very severe osteoporotic vertebral compression fractures: A randomized controlled study. Front Surg. 2022;9:1010042.
[21] ZHOU C, LIAO Y, HUANG S, et al. Effect of cement distribution type on clinical outcome after percutaneous vertebroplasty for osteoporotic vertebral compression fractures in the aging population. Front Surg. 2022;9:975832.
[22] 陆兆华,孙天泽,张警,等.不同入路椎体后凸成形术治疗骨质疏松性椎体压缩骨折[J].中国组织工程研究,2023,27(36):5834-5839.
[23] 童奕博,李明辉.骨质疏松性椎体骨折患者椎体成形后邻近椎体再发骨折的影响因素[J].中国组织工程研究,2024,28(8):1241-1246.
[24] DING JZ, KONG C, LI XY, et al. Different degeneration patterns of paraspinal muscles in degenerative lumbar diseases: a MRI analysis of 154 patients. Eur Spine J. 2022;31(3):764-773.
[25] WANG G, KARKI SB, XU S, et al. Quantitative MRI and X-ray analysis of disc degeneration and paraspinal muscle changes in degenerative spondylolisthesis. J Back Musculoskelet Rehabil. 2015;28(2):277-285.
[26] HODGES P, HOLM AK, HANSSON T, et al. Rapid atrophy of the lumbar multifidus follows experimental disc or nerve root injury. Spine (Phila Pa 1976). 2006;31(25):2926-2933.
[27] YOSHIHARA K, SHIRAI Y, NAKAYAMA Y, et al. Histochemical changes in the multifidus muscle in patients with lumbar intervertebral disc herniation. Spine (Phila Pa 1976). 2001;26(6):622-626.
[28] CHIOU SY, KOUTSOS E, GEORGIOU P, et al. Association between spectral characteristics of paraspinal muscles and functional disability in patients with low back pain: a cohort study. BMJ Open. 2018;8(2):e017091.
[29] CHANG DG, HEALEY RM, SNYDER AJ, et al. Lumbar Spine Paraspinal Muscle and Intervertebral Disc Height Changes in Astronauts After Long-Duration Spaceflight on the International Space Station. Spine (Phila Pa 1976). 2016;41(24):1917-1924.
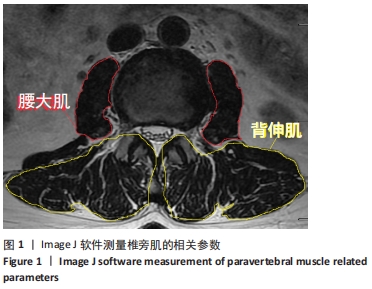
[30] FORTIN M, BATTIÉ MC. Quantitative paraspinal muscle measurements: inter-software reliability and agreement using OsiriX and ImageJ. Phys Ther. 2012;92(6):853-864.
[31] BATTAGLIA PJ, MAEDA Y, WELK A, et al. Reliability of the Goutallier classification in quantifying muscle fatty degeneration in the lumbar multifidus using magnetic resonance imaging. J Manipulative Physiol Ther. 2014;37(3):190-197.
[32] KALICHMAN L, HODGES P, LI L, et al. Changes in paraspinal muscles and their association with low back pain and spinal degeneration: CT study. Eur Spine J. 2010;19(7):1136-1144.
[33] NIEMELÄINEN R, BRIAND MM, BATTIÉ MC. Substantial asymmetry in paraspinal muscle cross-sectional area in healthy adults questions its value as a marker of low back pain and pathology. Spine (Phila Pa 1976). 2011;36(25):2152-2157.
|