[1] LOCHMANOVÁ G, JEDLIČKOVÁ L, POTĚŠIL D, et al. Potential biomarkers for early detection of acute graft-versus-host disease. Proteomics Clin Appl. 2012;6(7-8): 351-363.
[2] GATZA E, CHOI SW. Approaches for the prevention of graft-versus-host disease following hematopoietic cell transplantation. Int J Hematol Oncol. 2015;4(3):113-126.
[3] AOYAMA K, SAHA A, TOLAR J, et al. Inhibiting retinoic acid signaling ameliorates graft-versus-host disease by modifying T-cell differentiation and intestinal migration. Blood. 2013;122(12):2125-2134.
[4] GIEBEL S, GIORGIANI G, MARTINETTI M, et al. Low incidence of severe acute graft-versus-host disease in children given haematopoietic stem cell transplantation from unrelated donors prospectively matched for HLA class I and II alleles with high-resolution molecular typing. Bone Marrow Transplant. 2003;31(11):987-993.
[5] ROCHA V, WAGNER JE JR, SOBOCINSKI KA, et al. Graft-versus-host disease in children who have received a cord-blood or bone marrow transplant from an HLA-identical sibling. Eurocord and International Bone Marrow Transplant Registry Working Committee on Alternative Donor and Stem Cell Sources. N Engl J Med. 2000;342(25):1846-1854.
[6] KANOLD J, PAILLARD C, HALLE P, et al. Extracorporeal photochemotherapy for graft versus host disease in pediatric patients. Transfus Apher Sci. 2003;28(1):71-80.
[7] WASHINGTON K, JAGASIA M. Pathology of graft-versus-host disease in the gastrointestinal tract. Hum Pathol. 2009;40(7):909-917.
[8] PACZESNY S. Discovery and validation of graft-versus-host disease biomarkers. Blood. 2013;121(4):585-594.
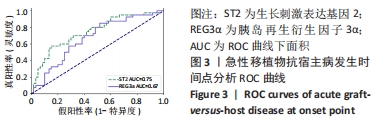
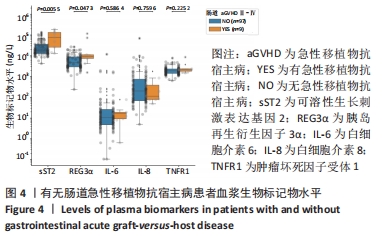
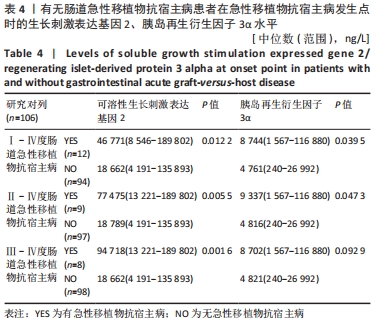
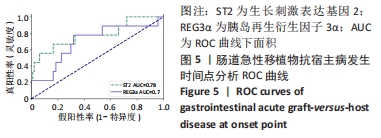
[9] VANDER LUGT MT, BRAUN TM, HANASH S, et al. ST2 as a marker for risk of therapy-resistant graft-versus-host disease and death. N Engl J Med. 2013;369(6): 529-539.
[10] FERRARA JL, HARRIS AC, GREENSON JK, et al. Regenerating islet-derived 3-alpha is a biomarker of gastrointestinal graft-versus-host disease. Blood. 2011;118(25): 6702-6708.
[11] PACZESNY S, BRAUN TM, LEVINE JE, et al. Elafin is a biomarker of graft-versus-host disease of the skin. Sci Transl Med. 2010;2(13):13ra2.
[12] TOUBAI T, TANAKA J, PACZESNY S, et al. Role of cytokines in the pathophysiology of acute graft-versus-host disease (GVHD): are serum/plasma cytokines potential biomarkers for diagnosis of acute GVHD following allogeneic hematopoietic cell transplantation (Allo-HCT)? Curr Stem Cell Res Ther. 2012;7(3):229-239.
[13] LEVINE JE, BRAUN TM, HARRIS AC, et al. A prognostic score for acute graft-versus-host disease based on biomarkers: a multicentre study. Lancet Haematol. 2015;2(1):e21-29.
[14] MAJOR-MONFRIED H, RENTERIA AS, PAWARODE A, et al. MAGIC biomarkers predict long-term outcomes for steroid-resistant acute GVHD. Blood. 2018; 131(25):2846-2855.
[15] 唐伦,颜红菊,高蕾,等.异基因造血干细胞移植患者血清生物标志物水平变化与aGHVD的关系[J].中国输血杂志,2016,29(6):598-601.
[16] 李桂芳.预测清髓性非血缘脐血移植后急性移植物抗宿主病发生风险以及预后的相关生物标记物研究[D].合肥:安徽医科大学,2015.
[17] SCHOEMANS HM, LEE SJ, FERRARA JL, et al. EBMT-NIH-CIBMTR Task Force position statement on standardized terminology & guidance for graft-versus-host disease assessment. Bone Marrow Transplant. 2018;53(11):1401-1415.
[18] MALONE FR, LEISENRING WM, STORER BE, et al. Prolonged anorexia and elevated plasma cytokine levels following myeloablative allogeneic hematopoietic cell transplant. Bone Marrow Transplant. 2007;40(8):765-772.
[19] HUESO T, COITEUX V, JONCQUEL CHEVALIER CURT M, et al. Citrulline and Monocyte-Derived Macrophage Reactivity before Conditioning Predict Acute Graft-versus-Host Disease. Biol Blood Marrow Transplant. 2017;23(6):913-921.
[20] PACZESNY S, KRIJANOVSKI OI, BRAUN TM, et al. A biomarker panel for acute graft-versus-host disease. Blood. 2009;113(2):273-278.
[21] BERGER M, SIGNORINO E, MURARO M, et al. Monitoring of TNFR1, IL-2Rα, HGF, CCL8, IL-8 and IL-12p70 following HSCT and their role as GVHD biomarkers in paediatric patients. Bone Marrow Transplant. 2013;48(9):1230-1236.
[22] CHOI SW, KITKO CL, BRAUN T, et al. Change in plasma tumor necrosis factor receptor 1 levels in the first week after myeloablative allogeneic transplantation correlates with severity and incidence of GVHD and survival. Blood. 2008;112(4): 1539-1542.
[23] MOLOFSKY AB, SAVAGE AK, LOCKSLEY RM. Interleukin-33 in Tissue Homeostasis, Injury, and Inflammation. Immunity. 2015;42(6):1005-1019.
[24] CHANG L, FRAME D, BRAUN T, et al. Engraftment syndrome after allogeneic hematopoietic cell transplantation predicts poor outcomes. Biol Blood Marrow Transplant. 2014;20(9):1407-1417.
[25] MCDONALD GB, TABELLINI L, STORER BE, et al. Plasma biomarkers of acute GVHD and nonrelapse mortality: predictive value of measurements before GVHD onset and treatment. Blood. 2015;126(1):113-120.
[26] REICHENBACH DK, SCHWARZE V, MATTA BM, et al. The IL-33/ST2 axis augments effector T-cell responses during acute GVHD. Blood. 2015;125(20):3183-3192.
[27] LAI Y, LI D, LI C, et al. The antimicrobial protein REG3A regulates keratinocyte proliferation and differentiation after skin injury. Immunity. 2012;37(1):74-84.
[28] TAKASHIMA S, KADOWAKI M, AOYAMA K, et al. The Wnt agonist R-spondin1 regulates systemic graft-versus-host disease by protecting intestinal stem cells. J Exp Med. 2011;208(2):285-294.
[29] YANG C,RAMADAN A, DAGUINDAU E, et al. Small Molecule ST2 Inhibitors Cause Reduction of Soluble ST2 and Improve Gvhd and Survival In Vivo. Blood. 2016;128(22):528.
|