中国组织工程研究 ›› 2020, Vol. 24 ›› Issue (24): 3834-3839.doi: 10.3969/j.issn.2095-4344.2750
• 人工假体 artificial prosthesis • 上一篇 下一篇
SuperPATH与传统后外侧入路全髋关节置换治疗老年股骨颈骨折的对比
胡正霞,兰 海,员 晋,李开南
- 成都大学附属医院骨科,四川省成都市 610081
Total hip arthroplasty for senile femoral neck fractures: SuperPATH approach versus traditional posterolateral approach
Hu Zhengxia, Lan Hai, Yuan Jin, Li Kainan
- Department of Orthopedics, Affiliated Hospital of Chengdu University, Chengdu 610081, Sichuan Province, China
摘要:

文题释义:
SuperPATH:即为supercapsular percutaneously assisted total hip arthroplasty的简称,上方关节囊经皮辅助全髋关节置换技术。该入路具有不切断外旋肌群并保留髋关节囊的特点,有利于患者术后早期下地活动,相对于其他手术入路,出现髋关节脱位的风险明显降低。
全髋关节置换:是采用人工髋关节替代自身髋关节,适用于终末期髋关节骨性关节炎和老年股骨颈骨折等,手术方法是切除自身的股骨头和股骨颈,将金属关节假体置入股骨近端和髋臼侧,使之替代人体髋关节进行活动。
背景:近年来全髋关节置换出现多种微创入路,其中CHOW等于2010年提出Superpath入路。该入路具有不切断外旋肌群并保留髋关节囊的特点,有利于患者术后早期下地活动,相对于其他手术入路,出现髋关节脱位的风险明显降低。
目的:对比分析SuperPATH入路与传统后外侧入路全髋关节置换治疗老年股骨颈骨折的近期疗效。
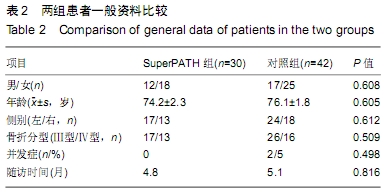
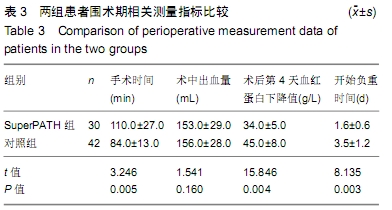
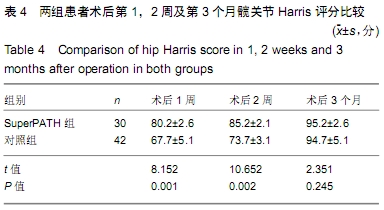
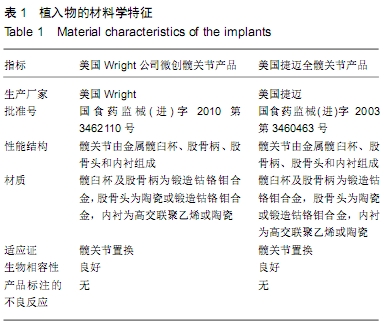
方法:回顾性分析2017年8月至2019年3月成都大学附属医院骨科治疗的72例65岁以上股骨颈骨折行全髋关节置换的患者,依据患者意愿分组,其中30例采用SuperPATH入路,42例采用传统后外侧入路。记录2组患者手术时间、术中失血量、术后第4天血红蛋白下降值及开始负重活动时间,于术后第1,2周及第3个月分别采用Harris评分评价患者髋关节功能恢复情况。
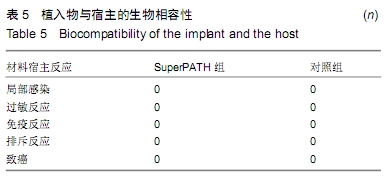
结果与结论:①所有患者均获得满意随访,随访时间3-6个月;②术后第2周所有患者均顺利出院,期间均无深静脉血栓形成、坐骨神经损伤、假体周围骨折、假体松动及假体周围感染等并发症发生,其中传统后外侧入路组有2例患者出现髋关节后脱位,均急诊在全麻下行手法牵引复位;③与对照组相比,SuperPATH组患者的手术时间更长,术后第4天血红蛋白下降值减小,开始负重活动时间较早,差异均有显著性意义(P < 0.01);但2组术中失血量比较差异无显著性意义(P > 0.05);④SuperPATH组术后第1,2周 Harris评分均高于对照组,差异均有显著性意义(P < 0.01);术后第3个月2组Harris评分差异无显著性意义(P > 0.05);⑤提示与后外侧入路相比,SuperPATH入路全髋关节置换治疗股骨颈骨折为微创手术,可有效减少手术创伤并加快术后髋关节功能恢复,减轻术后髋关节疼痛不适,降低髋关节脱位发生率;但由于手术难度大,学习曲线长,手术时间明显延长,导致术中出血量并无明显减少,由经验丰富的关节外科医生施行手术可有效降低并发症的发生。
ORCID: 0000-0002-9280-8802(胡正霞)
中国组织工程研究杂志出版内容重点:人工关节;骨植入物;脊柱;骨折;内固定;数字化骨科;组织工程
中图分类号: