[1] ATKIN L, BUĆKO Z, CONDE MONTERO E, et al. Implementing TIMERS: the race against hard-to-heal wounds. J Wound Care. 2019;23(Sup3a):S1-S50.
[2] DAS S, BAKER AB. Biomaterials and Nanotherapeutics for Enhancing Skin Wound Healing. Front Bioeng Biotechnol. 2016;4:82.
[3] SANTOS-VIZCAINO E, SALVADOR A, VAIRO C, et al. Overcoming the Inflammatory Stage of Non-Healing Wounds: In Vitro Mechanism of Action of Negatively Charged Microspheres (NCMs). Nanomaterials (Basel). 2020; 10(6):1108.
[4] YANG H. Progress in treatment of refractory wound and its challenges we are facing. Zhonghua Shao Shang Za Zhi. 2016;32(4):193-195.
[5] CHEN Q, DENG X, QIANG L, et al. Investigating the effects of walnut ointment on non-healing burn wounds. Burns. 2021;47(2):455-465.
[6] ZHAO D, XIAO J, QIANG L, et al. Walnut ointment promotes full-thickness burning wound healing: role of linoleic acid. Acta Cir Bras. 2022;37(9):e370902.
[7] CARDOSO C.R, FAVORETO S JR, OLIVEIRA LL, et al. Oleic acid modulation of the immune response in wound healing: a new approach for skin repair. Immunobiology. 2011;216(3):409-415.
[8] RODRIGUES HG, VINOLO MA, MAGDALON J, et al. Oral administration of oleic or linoleic acid accelerates the inflammatory phase of wound healing. J Invest Dermatol. 2012;132(1):208-215.
[9] GUIMARÃES D, CAVACO-PAULO A, NOGUEIRA E. Design of liposomes as drug delivery system for therapeutic applications. Int J Pharm. 2021;601:120571.
[10] DYMEK M, SIKORA E. Liposomes as biocompatible and smart delivery systems - the current state. Adv Colloid Interface Sci. 2022;309:102757.
[11] SAPKOTA R, DASH AK. Liposomes and transferosomes: a breakthrough in topical and transdermal delivery. Ther Deliv. 2021;12(2):145-158.
[12] CARITA AC, ELOY JO, CHORILLI M, et al. Recent Advances and Perspectives in Liposomes for Cutaneous Drug Delivery. Curr Med Chem. 2018;25(5):606-635.
[13] KIKUCHI IS, CARDOSO GALANTE RS, DUA K, et al. Hydrogel Based Drug Delivery Systems: A Review with Special Emphasis on Challenges Associated with Decontamination of Hydrogels and Biomaterials. Curr Drug Deliv. 2017;14(7):917-925.
[14] LIU K, WEI S, SONG L, et al. Conductive Hydrogels-A Novel Material: Recent Advances and Future Perspectives. J Agric Food Chem. 2020;68(28):7269-7280.
[15] TANG Q, DONG M, XU Z, et al. Red blood cell-mimicking liposomes loading curcumin promote diabetic wound healing. J Control Release. 2023;361:871-884.
[16] KANT V, GOPAL A, KUMAR D, et al. Topical pluronic F-127 gel application enhances cutaneous wound healing in rats. Acta Histochem. 2014;116(1):5-13.
[17] CHEN Q, ZHOU H, YANG Y, et al. Investigating the potential of Oxymatrine as a psoriasis therapy. Chem Biol Interact. 2017;271:59-66.
[18] GHLISSI Z, SAYARI N, KALLEL R, et al. Antioxidant, antibacterial, anti-inflammatory and wound healing effects of Artemisia campestris aqueous extract in rat. Biomed Pharmacother. 2016;84:115-122.
[19] KAROUD W, GHLISSI Z, KRICHEN F, et al. Oil from hake (Merluccius merluccius): Characterization, antioxidant activity, wound healing and anti-inflammatory effects. J Tissue Viability. 2020;29(2):138-147.
[20] BILGEN F, URAL A, KURUTAS EB, et al. The effect of oxidative stress and Raftlin levels on wound healing. Int Wound J. 2019;16(5):1178-1184.
[21] DENG X, CHEN Q, QIANG L, et al. Development of a Porcine Full-Thickness Burn Hypertrophic Scar Model and Investigation of the Effects of Shikonin on Hypertrophic Scar Remediation. Front Pharmacol. 2018;9:590.
[22] PIELESZ A, BINIAŚ D, SARNA E, et al. Active antioxidants in ex-vivo examination of burn wound healing by means of IR and Raman spectroscopies-Preliminary comparative research. Spectrochim Acta A Mol Biomol Spectrosc. 2017;173:924-930.
[23] MOREIRA E, BURGHI G, MANZANARES W. Update on metabolism and nutrition therapy in critically ill burn patients. Med Intensiva (Engl Ed). 2018; 42(5):306-316.
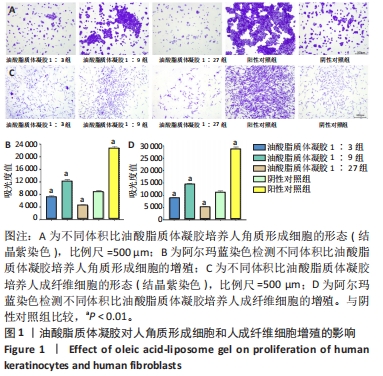
[24] AMIRI N, GOLIN AP, JALILI RB, et al. Roles of cutaneous cell-cell communication in wound healing outcome: An emphasis on keratinocyte-fibroblast crosstalk. Exp Dermatol. 2022;31(4):475-484.
[25] STUNOVA A, VISTEJNOVA L. Dermal fibroblasts-A heterogeneous population with regulatory function in wound healing. Cytokine Growth Factor Rev. 2018;39:137-150.
[26] KIRSNER RS, EAGLSTEIN WH. The wound healing process. Dermatol Clin. 1993;11(4):629-640.
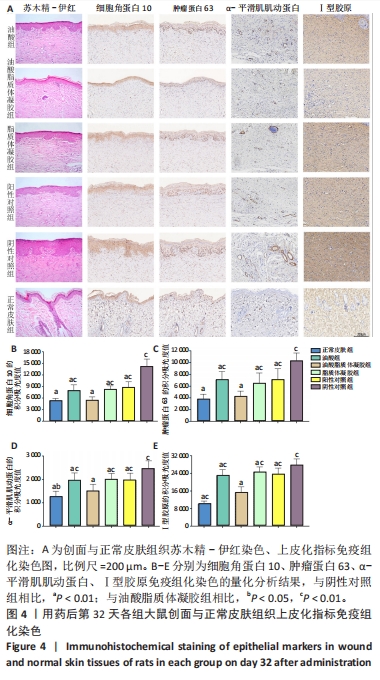
[27] OTA T, TAKEKOSHI S, TAKAGI T, et al. Notch signaling may be involved in the abnormal differentiation of epidermal keratinocytes in psoriasis. Acta Histochem Cytochem. 2014;47(4):175-183.
[28] KURINNA S, SELTMANN K, BACHMANN AL, et al. Interaction of the NRF2 and p63 transcription factors promotes keratinocyte proliferation in the epidermis. Nucleic Acids Res. 2021;49(7):3748-3763.
[29] JIANG Y, TSOI LC, BILLI AC, et al. Cytokinocytes: the diverse contribution of keratinocytes to immune responses in skin. JCI Insight. 2020;5(20):e142067.
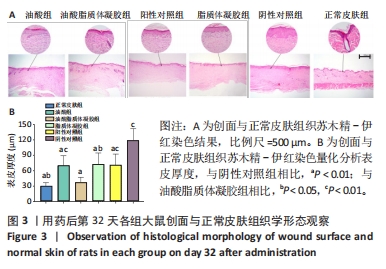
[30] XUE M, JACKSON CJ. Extracellular Matrix Reorganization During Wound Healing and Its Impact on Abnormal Scarring. Adv Wound Care(New Rochelle). 2015;4(3):119-136.
[31] REINKE JM, SORG H. Wound repair and regeneration. Eur Surg Res. 2012; 49(1):35-43.
[32] CARTHY JM, SUNDQVIST A, HELDIN A, et al. Tamoxifen Inhibits TGF-β-Mediated Activation of Myofibroblasts by Blocking Non-Smad Signaling Through ERK1/2. J Cell Physiol. 2015;230(12):3084-3092.
[33] HINZ B. Formation and function of the myofibroblast during tissue repair. J Invest Dermatol. 2007;127(3):526-537.
[34] HINZ B. The role of myofibroblasts in wound healing. Curr Res Transl Med. 2016;64(4):171-177.
[35] SULAIMAN M, SALEM RA, RAGHAVANKUTTY M, et al. Sulfated polysaccharide ascophyllan from Padina tetrastromatica enhances healing of burn wounds by ameliorating inflammatory responses and oxidative damage. Mol Biol Rep. 2020;47(11):8701-8710.
[36] GHLISSI Z, KALLEL R, SILA A, et al. Globularia alypum methanolic extract improves burn wound healing process and inflammation in rats and possesses antibacterial and antioxidant activities. Biomed Pharmacother. 2016;84:1488-1495.
[37] WU YK, CHENG NC, CHENG CM. Biofilms in Chronic Wounds: Pathogenesis and Diagnosis. Trends Biotechnol. 2019;37(5):505-517.
[38] BERNER T, NAKAHARA K, KOBAYASHI E, et al. Investigating the effect of antiseptic solution on the release of interleukin-6 and transforming growth factor beta 1 from human gingival fibroblasts using wound healing assays. J Oral Sci. 2020;62(3):293-297.
[39] DENG L, DU C, SONG P, et al. The Role of Oxidative Stress and Antioxidants in Diabetic Wound Healing. Oxid Med Cell Longev. 2021;2021:8852759.
[40] PARIHAR A, PARIHAR MS, MILNER S, et al. Oxidative stress and anti-oxidative mobilization in burn injury. Burns. 2008;34(1):6-17.
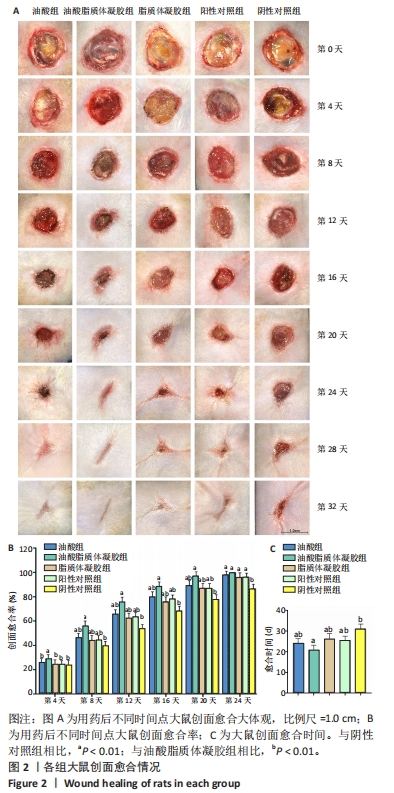
[41] NUNAN R, HARDING KG, MARTIN P. Clinical challenges of chronic wounds: searching for an optimal animal model to recapitulate their complexity. Dis Model Mech. 2014;7(11):1205-1213.
[42] HESKETH M, SAHIN KB, WEST ZE, et al. Macrophage Phenotypes Regulate Scar Formation and Chronic Wound Healing. Int J Mol Sci. 2017;18(7):1545.
[43] PATEL S, MAHESHWARI A, CHANDRA A. Biomarkers for wound healing and their evaluation. J Wound Care. 2016;25(1):46-55.
[44] SMITH JR, BOLTON ER, DWINELL MR. The Rat: A Model Used in Biomedical Research. Methods Mol Biol. 2019;2018:1-41.
[45] MI XJ, LE HM, LEE S, et al. Silymarin-Functionalized Selenium Nanoparticles Prevent LPS-Induced Inflammatory Response in RAW264.7 Cells through Downregulation of the PI3K/Akt/NF-κB Pathway. ACS Omega. 2022;7(47): 42723-42732.
[46] GUO W, QIU W, AO X, et al. Low-concentration DMSO accelerates skin wound healing by Akt/mTOR-mediated cell proliferation and migration in diabetic mice. Br J Pharmacol. 2020;177(14):3327-3341. |