[1] GREGSON C, ARMSTRONG DJ, BOWDEN J, et al. UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos. 2022;17(1):1-46.
[2] CURTIS EM, Reginster JY, Al-Daghri N, et al. Management of patients at very high risk of osteoporotic fractures through sequential treatments. Aging Clin Exp Res. 2022;34:695-714.
[3] ZHANG W, GAO R, RONG X, et al. Immunoporosis: Role of immune system in the pathophysiology of different types of osteoporosis. Front Endocrinol (Lausanne). 2022;13:965258.
[4] EASTELL R, O’NEILL TW, HOFBAUER LC, et al. Postmenopausal osteoporosis. Nat Rev Dis Primers. 2016;2(1):1-16.
[5] WANG A, ZHANG H, LI G, et al. Deciphering core proteins of osteoporosis with iron accumulation by proteomics in human bone. Front Endocrinol (Lausanne). 2022;13:961903.
[6] CRANDALL CJ, VASAN S, LACROIX A, et al. Bone turnover markers are not associated with hip fracture risk: a case‐control study in the Women’s Health Initiative. J Bone Miner Res. 2018;33(7):1199-1208.
[7] BROWN JP. Long-term treatment of postmenopausal osteoporosis. Endocrinol Metab (Seoul). 2021;36(3):544.
[8] SŁUPSKI W, JAWIEŃ P, NOWAK B. Botanicals in postmenopausal osteoporosis. Nutrients. 2021;13(5):1609.
[9] KERSCHAN-SCHINDL K, HACKL M, BOSCHITSCH E, et al. Diagnostic performance of a panel of mirnas (osteomir) for osteoporosis in a cohort of postmenopausal women. Calcif Tissue Int. 2021;108(6):725-737.
[10] WANG G, ZHANG L, YAN C, et al. Overexpression of miR125b Promotes Osteoporosis Through miR-125b-TRAF6 Pathway in Postmenopausal Ovariectomized Rats. Diabetes Metab Syndr Obes. 2021;14:671.
[11] DE MARTINIS M, GINALDI L, ALLEGRA A, et al. The osteoporosis/microbiota linkage: the role of miRNA. Int J Mol Sci. 2020;21(23):8887.
[12] ZHAO Y, JIA L, ZHENG Y, et al. Involvement of noncoding RNAs in the differentiation of osteoclasts. Stem Cells Int. 2020;2020:4813140.
[13] AI L, YI W, CHEN L, et al. Xian-Ling-Gu-Bao protects osteoporosis through promoting osteoblast differentiation by targeting miR-100-5p/KDM6B/RUNX2 axis. In Vitro Cell Dev Biol Anim. 2021;57:3-9.
[14] WANG R, ZHANG M, HU Y, et al. MiR-100-5p inhibits osteogenic differentiation of human bone mesenchymal stromal cells by targeting TMEM135. Hum Cell. 2022;35(6):1671-1683.
[15] LI J, LI Y, WANG S, et al. miR-101-3p/Rap1b signal pathway plays a key role in osteoclast differentiation after treatment with bisphosphonates. BMB Rep. 2019; 52(9):572.
[16] HUANG AY, XIONG Z, LIU K, et al. Identification of kaempferol as an OSX upregulator by network pharmacology-based analysis of qianggu Capsule for osteoporosis. Front Pharmacol. 2022;13:1011561.
[17] TANG Y, PENG B, LIU J, et al. Systemic immune-inflammation index and bone mineral density in postmenopausal women: A cross-sectional study of the national health and nutrition examination survey (NHANES) 2007-2018. Front Immunol. 2022;13:975400.
[18] XU Y, YAN H, ZHANG X, et al. Roles of Altered Macrophages and Cytokines: Implications for Pathological Mechanisms of Postmenopausal Osteoporosis, Rheumatoid Arthritis, and Alzheimer’s Disease. Front Endocrinol (Lausanne). 2022;13:876269.
[19] SRIVASTAVA RK, SAPRA L. The Rising Era of “Immunoporosis”: Role of Immune System in the Pathophysiology of Osteoporosis. J Inflamm Res. 2022;15: 1667.
[20] WU D, CLINE-SMITH A, SHASHKOVA E, et al. T-cell mediated inflammation in postmenopausal osteoporosis. Front Immunol. 2021;12:2413.
[21] CHARATCHAROENWITTHAYA N, KHOSLA S, ATKINSON EJ, et al. Effect of blockade of TNF‐α and interleukin‐1 action on bone resorption in early postmenopausal women. J Bone Miner Res. 2007;22(5):724-729.
[22] YANG K, CAO F, XUE Y, et al. Three Classes of Antioxidant Defense Systems and the Development of Postmenopausal Osteoporosis. Front Physiol. 2022;13:840293.
[23] LIANG B, BURLEY G, LIN S, et al. Osteoporosis pathogenesis and treatment: existing and emerging avenues. Cell Mol Biol Lett. 2022;27:72.
[24] BHATNAGAR A, KEKATPURE AL. Postmenopausal Osteoporosis: A Literature Review. Cureus. 2022;14:e29367.
[25] LIU T, HUANG J, XU D, et al. Identifying a possible new target for diagnosis and treatment of postmenopausal osteoporosis through bioinformatics and clinical sample analysis. Ann Transl Med. 2021;9(14):1154.
[26] SHAHRIARPOUR Z, NASRABADI B, HEJRI-ZARIFI S, et al. Oxidative balance score and risk of osteoporosis among postmenopausal Iranian women. Arch Osteoporos. 2021;16(1):1-10.
[27] XU J, LI M, PEI W, et al. Reduced Circulating Levels of miR-491-5p and miR-485-3p Are Associated with the Occurrence of Vertebral Fractures in Postmenopausal Women with Osteoporosis. Genet Res (Camb). 2022;2022:3838126.
[28] PALA E, DENKÇEKEN T. Differentially expressed circulating miRNAs in postmenopausal osteoporosis: a meta-analysis. Biosci Rep. 2019;39(5):BSR20190667.
[29] JOHN AA, XIE J, YANG YS, et al. AAV-mediated delivery of osteoblast/osteoclast-regulating miRNAs for osteoporosis therapy. Mol Ther Nucleic Acids. 2022;29: 296-311.
[30] SHI H, JIANG X, XU C, et al. MicroRNAs in Serum Exosomes as Circulating Biomarkers for Postmenopausal Osteoporosis. Front Endocrinol (Lausanne). 2022; 13:819056.
[31] HAN Y, YANG Q, HUANG Y, et al. Long non-coding RNA SNHG5 promotes the osteogenic differentiation of bone marrow mesenchymal stem cells via the miR-212-3p/GDF5/SMAD pathway. Stem Cell Res Ther. 2022;13:130.
[32] GRUNDMANN S, HANS FP, KINNIRY S, et al. MicroRNA-100 regulates neovascularization by suppression of mammalian target of rapamycin in endothelial and vascular smooth muscle cells. Circulation. 2011;123(9):999-1009.
[33] Verdelli C, Sansoni V, Perego S, et al. Circulating fractures-related microRNAs distinguish primary hyperparathyroidism-related from estrogen withdrawal-related osteoporosis in postmenopausal osteoporotic women: A pilot study. Bone. 2020;137:115350.
[34] WANG R, LU A, LIU W, et al. Searching for valuable differentially expressed miRNAs in postmenopausal osteoporosis by RNA sequencing. J Obstet Gynaecol Res. 2020;46:1183-1192.
[35] CARTHEW J, DONDERWINKEL I, SHRESTHA S, et al. In situ miRNA delivery from a hydrogel promotes osteogenesis of encapsulated mesenchymal stromal cells. Acta Biomater. 2020;101:249-261.
[36] XIANG J, FU H Q, XU Z, et al. lncRNA SNHG1 attenuates osteogenic differentiation via the miR 101/DKK1 axis in bone marrow mesenchymal stem cells. Mol Med Rep. 2020;22(5):3715-3722.
[37] WU P, JIAO F, HUANG H, et al. Morinda officinalis polysaccharide enable suppression of osteoclastic differentiation by exosomes derived from rat mesenchymal stem cells. Pharm Biol. 2022;60(1):1303-1316.
[38] AIBAR-ALMAZAN A, VOLTES-MARTINEZ A, CASTELLOTE-CABALLERO Y, et al. Current Status of the Diagnosis and Management of Osteoporosis. Int J Mol Sci. 2022;23(16):9465.
[39] DAI Z, WEI G. Inhibition of miRNA-100 facilitates bone regeneration defects of mesenchymal stem cells in osteoporotic mice through the protein kinase B pathway. Bioengineered. 2022;13(1):963-973.
[40] ZOU W, IZAWA T, ROHATGI N, et al. ThPOK Inhibits Osteoclast Formation Via NFATc1 Transcription and Function. JBMR Plus. 2022;6:e10613.
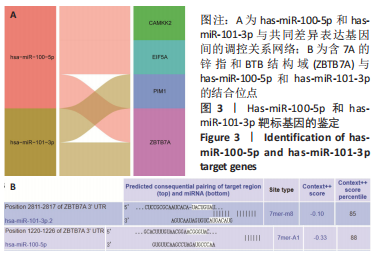
[41] RAMOS PITTOL JM, ORUBA A, MITTLER G, et al. Zbtb7a is a transducer for the control of promoter accessibility by NF-kappa B and multiple other transcription factors. PLoS Biol. 2018;16:e2004526.
[42] CONSTANTINOU C, SPELLA M, CHONDROU V, et al. The multi-faceted functioning portrait of LRF/ZBTB7A. Hum Genomics. 2019;13(1):1-14.
|