中国组织工程研究 ›› 2021, Vol. 25 ›› Issue (13): 1993-1998.doi: 10.3969/j.issn.2095-4344.3510
• 造血干细胞 hematopoietic stem cells • 上一篇 下一篇
自体造血干细胞移植治疗恶性淋巴瘤的疗效及影响因素
曹琳琳,丁凯阳,宋 浩,吴国林,胡茂贵,范丹丹,周晨阳,王翠翠,封媛媛
- 中国科学技术大学附属第一医院西区血液科,安徽省合肥市 230000
Efficacy and influencing factors of autologous hematopoietic stem cell transplantation in the treatment of malignant lymphoma
Cao Linlin, Ding Kaiyang, Song Hao, Wu Guolin, Hu Maogui, Fan Dandan, Zhou Chenyang, Wang Cuicui, Feng Yuanyuan
- Department of Hematology, Western District, The First Affiliated Hospital of University of Science and Technology of China, Hefei 230000, Anhui Province, China
摘要:
文题释义:
自体造血干细胞移植:首先在疾病缓解期采集患者自身的造血干细胞,进行体外冻存,待患者经过高剂量化疗或联合全身照射或全淋巴结照射(即预处理治疗)后再将其回输至患者体内,使患者的骨髓造血和免疫功能得以恢复和重建,从而在保证患者安全的前提下,最大限度地杀伤肿瘤细胞,提高治疗效果,显著延长疾病无进展生存期及总生存期,改善患者预后及生活质量,是淋巴瘤整体治疗中不可替代的重要治疗手段。美国血液和骨髓移植学会(ASBMT)、欧洲血液和骨髓移植组(EBMT)指南及国内《造血干细胞移植治疗淋巴瘤中国专家共识(2018版)》均推荐自体造血干细胞移植用于淋巴瘤的一线巩固治疗和复发后挽救治疗。
复发难治性淋巴瘤:淋巴瘤为一组起源于淋巴结或其他淋巴组织的异质性血液系统恶性肿瘤,包括霍奇金淋巴瘤和非霍奇金淋巴瘤,经过标准一线方案治疗,超过60%患者的生存期显著提高,然而仍有30%-40%患者出现疾病复发或难治,预后较差,如何延长复发难治性弥漫性大B细胞淋巴瘤患者的生存期、改善患者预后已成为国内外的研究热点。通过对基因表达谱、耐药分子机制等深入研究,化疗新方案及新药联合自体造血干细胞移植为改善此类患者的不良预后提供了新思路和新方向。
背景:针对淋巴瘤的治疗方案包括化学治疗、局部放射治疗、自体外周血造血干细胞移植及细胞免疫治疗等。大剂量化疗联合自体造血干细胞移植能明显延长患者的生存时间,改善预后,被推荐为复发难治性和(或)高侵袭性淋巴瘤的一线治疗方案。
目的:分析大剂量化疗联合自体造血干细胞移植治疗恶性淋巴瘤患者的临床特征及生存预后因素等,以期提高临床医师对自体造血干细胞移植治疗淋巴瘤的认识。
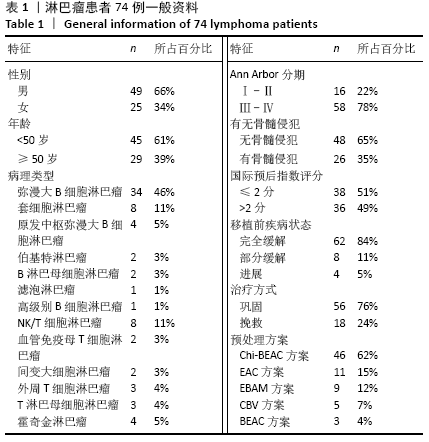
方法:回顾性分析2015年10月至2020年3月就诊于中国科学技术大学附属第一医院西区血液科移植病房,行大剂量化疗联合自体造血干细胞移植治疗的74例淋巴瘤患者的临床资料,评价自体造血干细胞移植治疗淋巴瘤的疗效和影响预后的相关因素。
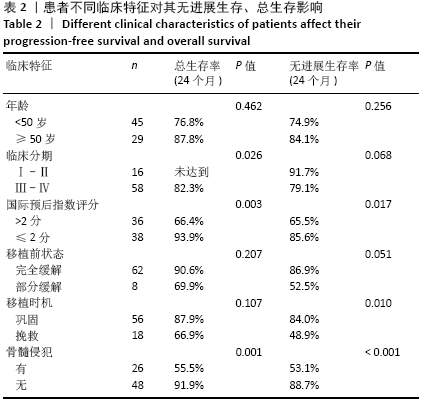
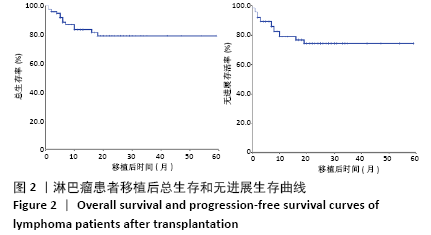
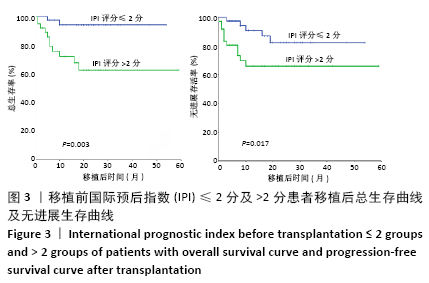
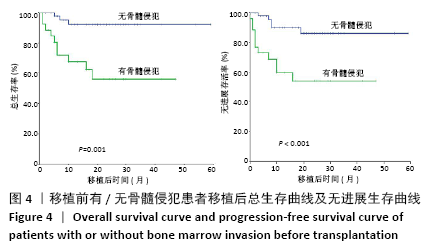
结果与结论:①随访截至于 2020-05-15,确诊至移植中位时间为8(3-83)个月,中位随访时间为17(2-59)个月;②所有患者移植后均获得造血重建,粒细胞植入中位时间为+10(+8至+17) d,血小板植入中位时间为+12(+9至+22) d;③移植后无进展生存60例,复发13例,复发患者中死亡11例,1例于移植后11个月因肺部感染死亡;④4例移植前为进展期患者均于移植后7个月内因原发病进展死亡;⑤74例患者接受造血干细胞移植后2年总生存率为78.5%,2年无进展生存率为75.8%;移植前国际预后指数≤2分及>2分患者移植后2年总生存分别为93.9%,66.4%(P=0.003),2年无进展生存分别为85.6%,65.5%(P=0.017);⑥移植前有骨髓侵犯及无骨髓侵犯患者移植后2年总生存率分别为55.5%,91.9 %(P=0.001);2年无进展生存率分别为53.1%,88.7%(P < 0.001);⑦临床分期Ⅰ、Ⅱ期患者2年总生存率优于临床分期Ⅲ、Ⅳ期患者(100% vs. 82.5%,P=0.026);一线巩固治疗患者2年无进展生存率优于挽救治疗组(84% vs. 48.9%,P=0.01);患者年龄、移植前缓解程度对无进展生存和总生存影响的差异均无显著性意义;⑧结果表明,大剂量化疗联合自体造血干细胞移植可明显改善淋巴瘤患者生存及预后,且安全性高,可作为淋巴瘤的一种安全有效的治疗方式。国际预后指数分值、有无骨髓侵犯、移植时机选择及原发病分期为影响患者预后的因素。
https://orcid.org/0000-0002-7035-0474(曹琳琳)
中国组织工程研究杂志出版内容重点:干细胞;骨髓干细胞;造血干细胞;脂肪干细胞;肿瘤干细胞;胚胎干细胞;脐带脐血干细胞;干细胞诱导;干细胞分化;组织工程
中图分类号: