中国组织工程研究 ›› 2019, Vol. 23 ›› Issue (26): 4181-4186.doi: 10.3969/j.issn.2095-4344.1357
• 细胞外基质材料 extracellular matrix materials • 上一篇 下一篇
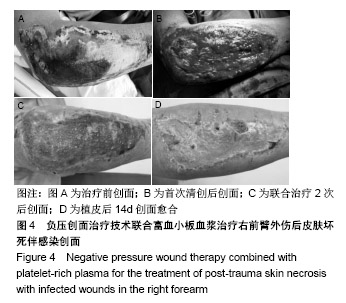
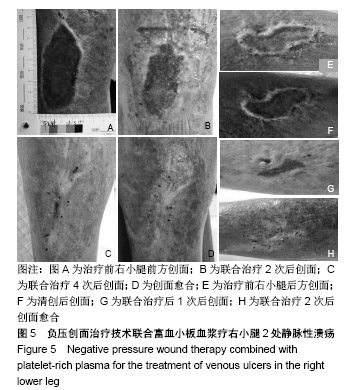
负压创面治疗技术联合富血小板血浆治疗慢性难愈性创面:加速创面的再上皮化及愈合率
杨 彪1,王 珊2,张 岩1,梁春雨1
- 1华北理工大学附属医院,河北省唐山市 063000;2邢台医专第二附属医院,河北省邢台市 054000
Treatment of chronic refractory wounds with negative pressure wound therapy and platelet-rich plasma: accelerating the re-epithelialization of wounds and increasing
Yang Biao1, Wang Shan2, Zhang Yan1, Liang Chunyu1
- 1North China University of Science and Technology Affiliated Hospital, Tangshan 063000, Hebei Province, China; 2the Second Affiliated Hospital of Xingtai Medical College, Xingtai 054000, Hebei Province, China
摘要:
文章快速阅读:
.jpg)
文题释义:
慢性难愈性创面:目前对于慢性难愈性创面的具体定义尚未达成共识,国际创伤愈合学会定义慢性难愈性创面为无法通过正常、有序、及时的修复过程而造成的;或者是经过修复而没有恢复解剖和功能上完整状态的伤口。
富血小板血浆(PRP):是血小板浓缩物,一种用于刺激和加速组织愈合的新型生物技术,其生物学效应主要归因于其中的血小板分泌体和血浆信号蛋白等成分,富血小板血浆可在不同的病理微环境下,通过不同的再生机制,包括止血、炎症、血管生成和细胞外基质的合成等促进创面愈合,缩短创面愈合的时间。
背景:负压创面治疗技术已被证实是加速各种急慢性创面愈合的有效方法。富血小板血浆是一种用于刺激和加速组织愈合的生物技术。
目的:对比分析应用负压创面治疗技术联合富血小板血浆治疗与单纯应用负压创面治疗慢性难愈性创面中的临床疗效。
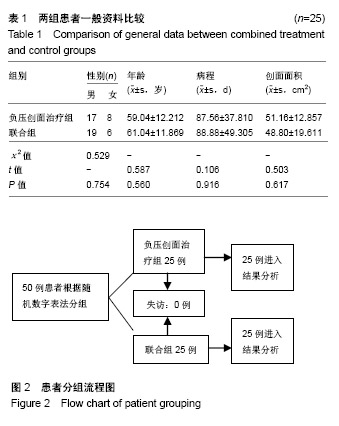
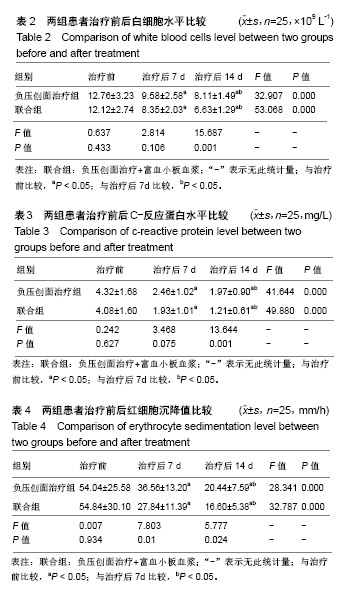
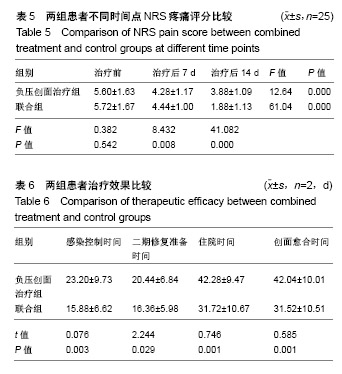
方法:研究经华北理工大学附属医院伦理委员会批准,所有入选患者及家属均签署了知情同意书。50例慢性难愈性创面患者按照随机数字表法分为负压创面治疗组25例和联合组25例。负压创面治疗组患者清创后行封闭负压吸引治疗,联合组患者清创后先以富血小板血浆凝胶覆盖创面然后再同负压创面治疗组患者行封闭负压吸引治疗。2组负压值均设定在-9.31至-39.9 kPa,采用持续吸引模式治疗,每7 d更换敷料,视创面愈合情况进行皮肤移植治疗。记录两组患者治疗前及治疗第7,14天的分泌物细菌培养结果的变化情况及白细胞、C-反应蛋白水平、红细胞沉降率水平,比较2组细菌转阴率、NRS疼痛评分、二期修复准备时间、创面愈合时间和住院时间。
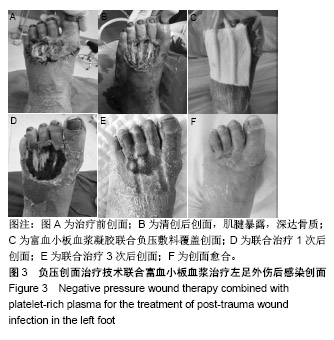
结果与结论:①2组患者治疗后7 d各项炎症因子水平比较差异无统计学意义(P > 0.05);②治疗后14 d联合组各项炎症指标水平、细菌转阴率、感染控制时间均显著低于单纯负压创面治疗组(P < 0.05);③治疗后2组患者疼痛评分在不同的时间点呈下降趋势(P < 0.05),治疗后14 d联合组患者疼痛评分较单纯负压创面治疗组显著降低(P < 0.05);④联合组二期修复手术所需时间、创面愈合时间、住院时间均显著优于单纯负压创面治疗组(P < 0.05);⑤所有患者出院后均获得随访,时间1-3个月,2组患者创面均无复发;⑥负压创面治疗联合富血小板血浆凝胶较单纯负压创面治疗慢性难愈性创面有更好地抑菌效果,能有效缩短创面床准备时间以及创面愈合时间,加速创面的再上皮化、提高创面愈合率,缓解患者疼痛。
中图分类号:
.jpg)
.jpg)