| [1] Cote P, van der Velde G, Cassidy JD, et al. The burden and determinants of neck pain in workers: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. J Manipulative Physiol Ther. 2009;32(2 Suppl): S70-86.[2] Cote P, Kristman V, Vidmar M, et al. The prevalence and incidence of work absenteeism involving neck pain: a cohort of Ontario lost-time claimants. J Manipulative Physiol Ther. 2009;32(2 Suppl): S219-226.[3] Mizutani J, Verma K, Endo K, et al. Global Spinal Alignment in Cervical Kyphotic Deformity: The Importance of Head Position and Thoracolumbar Alignment in the Compensatory Mechanism. Neurosurgery. 2017.[4] Merrill RK, Kim JS, Leven DM, et al. Beyond pelvic incidence-lumbar lordosis mismatch: the importance of assessing the entire spine to achieve global sagittal alignment. Global Spine J. 2017;7(6): 536-542.[5] Nordin M, Carragee EJ, Hogg-Johnson S, et al. Assessment of neck pain and its associated disorders: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. J Manipulative Physiol Ther. 2009;32(2 Suppl): S117-140.[6] Kumagai G, Ono A, Numasawa T, et al. Association between roentgenographic findings of the cervical spine and neck symptoms in a Japanese community population. J Orthop Sci. 2014;19(3): 390-397.[7] Grob D, Frauenfelder H, Mannion AF. The association between cervical spine curvature and neck pain. Eur Spine J. 2007;16(5): 669-678[8] Beltsios M, Savvidou O, Mitsiokapa EA, et al. Sagittal alignment of the cervical spine after neck injury. Eur J Orthop Surg Traumatol. 2013;23 Suppl 1:S47-51.[9] Singhatanadgige W, Kang DG, Luksanapruksa P, et al. Correlation and reliability of cervical sagittal alignment parameters between lateral cervical radiograph and lateral whole-body EOS stereoradiograph. Global Spine J. 2016;6(6): 548-554.[10] Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine. 2013; 19(2): 141-159.[11] Tsunoda D, Iizuka Y, Iizuka H, et al. Associations between neck and shoulder pain (called katakori in Japanese) and sagittal spinal alignment parameters among the general population. J Orthop Sci. 2013;18(2): 216-219.[12] Wang K, Deng Z, Li Z, et al. The Influence of Natural Head Position on the Cervical Sagittal Alignment. J Healthc Eng. 2017.[13] Cote P, Cassidy JD, Carroll LJ, et al. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain. 2004;112(3): 267-273.[14] Oshima Y, Takeshita K, Taniguchi Y, et al. Effect of preoperative sagittal balance on cervical laminoplasty outcomes. Spine (Phila Pa 1976). 2016;41(21): E1265-E1270.[15] Patwardhan AG, Khayatzadeh S, Havey RM, et al. Cervical sagittal balance: a biomechanical perspective can help clinical practice. Eur Spine J. 2017.[16] Harrison DE, Harrison DD, Janik TJ, et al. Comparison of axial and flexural stresses in lordosis and three buckled configurations of the cervical spine. Clin Biomech (Bristol, Avon). 2001;16(4): 276-284.[17] Dulhunty J. Evaluation of axial and flexural stresses in the vertebral body cortex and trabecular bone in lordosis and two sagittal cervical translation configurations with an elliptical shell model. J Manipulative Physiol Ther. 2003;26(9): 608-612.[18] Kwon TH, Park YK, Moon HJ. The relationship between neck pain and cervical alignment in young female nursing staff. J Korean Neurosurg Soc. 2015;58(3): 231-235.[19] Lippa L, Lippa L, Cacciola F. Loss of cervical lordosis: What is the prognosis? J Craniovertebr Junction Spine. 2017;8(1): 9-14.[20] Christensen ST, Hartvigsen J. Spinal curves and health: a systematic critical review of the epidemiological literature dealing with associations between sagittal spinal curves and health. J Manipulative Physiol Ther. 2008;31(9): 690-714.[21] Harrison DE, Harrison DD, Betz JJ, et al. Increasing the cervical lordosis with chiropractic biophysics seated combined extension-compression and transverse load cervical traction with cervical manipulation: nonrandomized clinical control trial. J Manipulative Physiol Ther. 2003;26(3): 139-151.[22] 任龙喜,何玉宝,郭函,等.颈部疼痛程度与颈椎曲度相关性的临床观察[J].中国脊柱脊髓杂志,2011,21(9):750-753.[23] Harrison DE, Cailliet R, Harrison DD, et al. A new 3-point bending traction method for restoring cervical lordosis and cervical manipulation: a nonrandomized clinical controlled trial. Arch Phys Med Rehabil. 2002;83(4): 447-453.[24] Protopsaltis TS, Scheer JK, Terran JS, et al. How the neck affects the back: changes in regional cervical sagittal alignment correlate to HRQOL improvement in adult thoracolumbar deformity patients at 2-year follow-up. J Neurosurg Spine. 2015;23(2): 153-158.[25] Diebo BG, Varghese JJ, Lafage R, et al. Sagittal alignment of the spine: What do you need to know? Clin Neurol Neurosurg. 2015;139:295-301.[26] Yu M, Silvestre C, Mouton T, et al. Analysis of the cervical spine sagittal alignment in young idiopathic scoliosis: a morphological classification of 120 cases. Eur Spine J. 2013;22(11): 2372-2381.[27] Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010;10(11): 994-998.[28] Lee SH, Kim KT, Seo EM, et al. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech. 2012;25(2): E41-47.[29] 赵文奎,于淼,韦峰,等.无症状成人颈椎矢状位曲度分析及其与全脊柱矢状位参数的关系[J].中国脊柱脊髓杂志,2015,25(3): 231-238.[30] Lee CS, Chung SS, Kang KC, et al. Normal patterns of sagittal alignment of the spine in young adults radiological analysis in a Korean population. Spine (Phila Pa 1976).2011;36(25): E1648-1654. |
.jpg)
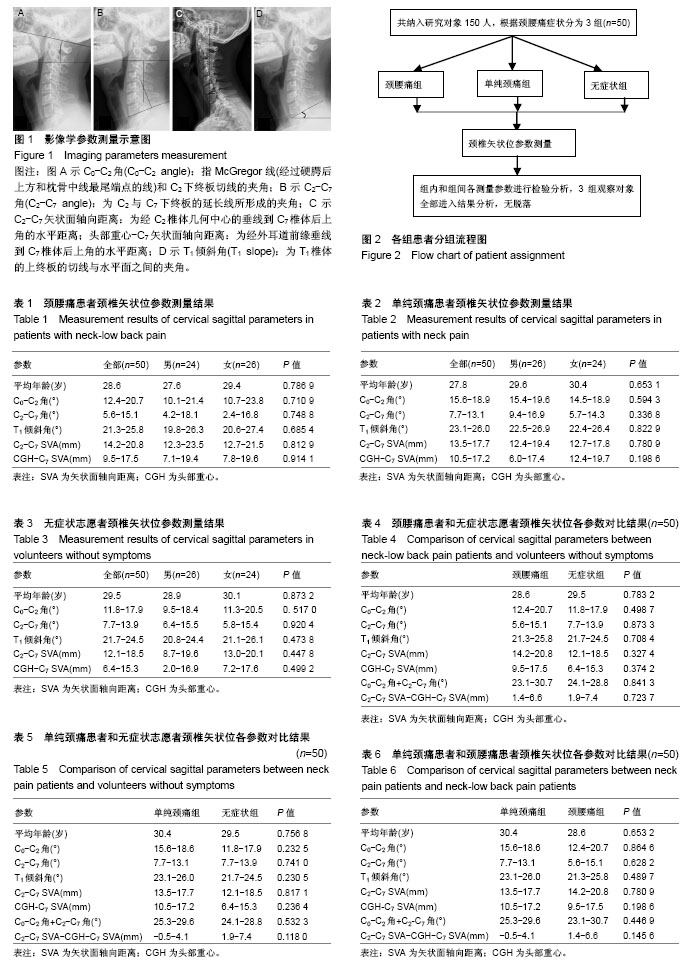
.jpg)