[1] 朱汉民,王松,肖文琳,等.线粒体自噬调控骨代谢[J].中国组织工程研究, 2025,29(8):1676-1683.
[2] CHENG K, GUO Q, YANG W, et al. Mapping Knowledge Landscapes and Emerging Trends of the Links Between Bone Metabolism and Diabetes Mellitus: A Bibliometric Analysis From 2000 to 2021. Front Public Health. 2022;10:918483.
[3] 郭曹培,程飘涛,杨成兵,等.骨免疫与骨代谢[J].中国组织工程研究,2024, 28(14):2261-2266.
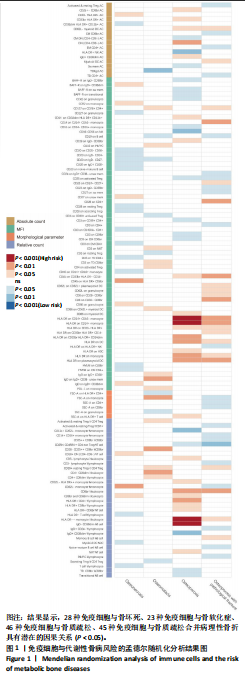
[4] CAO RR, YU XH, XIONG MF, et al. The immune factors have complex causal regulation effects on bone mineral density. Front Immunol. 2022;13:959417.
[5] ZHENG J, YAO Z, XUE L, et al. The role of immune cells in modulating chronic inflammation and osteonecrosis. Front Immunol. 2022;13:1064245.
[6] CHAROENNGAM N. Vitamin D and Rheumatic Diseases: A Review of Clinical Evidence. Int J Mol Sci. 2021;22(19):10659.
[7] FISCHER V, HAFFNER-LUNTZER M. Interaction between bone and immune cells: Implications for postmenopausal osteoporosis. Semin Cell Dev Biol. 2022;123:14-21.
[8] AURORA R, VEIS D. Does Aging Activate T-cells to Reduce Bone Mass and Quality? Curr Osteoporos Rep. 2022;20(5):326-333.
[9] EPSLEY S, TADROS S, FARID A, et al. The Effect of Inflammation on Bone. Front Physiol. 2021;11:511799.
[10] Orrù V, Steri M, Sidore C, et al. Complex genetic signatures in immune cells underlie autoimmunity and inform therapy. Nat Genet. 2020;52(10):1036-1045.
[11] KURKI MI, KARJALAINEN J, PALTA P, et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature. 2023;613(7944):508-518.
[12] SKRIVANKOVA VW, RICHMOND RC, WOOLF BAR, et al. Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization: The STROBE-MR Statement. JAMA. 2021;326(16):1614-1621.
[13] EMDIN CA, KHERA AV, KATHIRESAN S. Mendelian Randomization. JAMA. 2017; 318(19):1925-1926.
[14] LYU F, WANG L, JIA Y, et al. Analysis of Zinc and Stromal Immunity in Disuse Osteoporosis: Mendelian Randomization and Transcriptomic Analysis. Orthop Surg. 2023;15(11):2947-2959.
[15] 陈天鑫,张智龙,朱瑜琪,等.恶性肿瘤与骨密度因果关系的双向两样本孟德尔随机化研究[J].现代预防医学,2023,50(18):3276-3280+3287.
[16] 陈天鑫,董婷婷,李妍,等.孟德尔随机化分析血液代谢物与肌少症相关特征的因果关系[J].中国组织工程研究,2024,28(27):4288-4292.
[17] FEIGE J, MOSER T, AKGÜN K, et al. Repeated iv anti-CD20 treatment in multiple sclerosis: Long-term effects on peripheral immune cell subsets. Ann Clin Transl Neurol. 2024;11(2):450-465.
[18] JAVELOT MJ, SERGHERAERT J, AGBO-GODEAU S, et al. Rituximab as a trigger factor of medication-related osteonecrosis of the jaw. A case report. J Stomatol Oral Maxillofac Surg. 2020;121(3):300-304.
[19] KERIBIN P, GUERROT D, JARDIN F, et al. Osteonecrosis of the Jaw in a Patient Presenting With Post-Transplantation Lymphoproliferative Disorder Treated With Rituximab: A Case Report. J Oral Maxillofac Surg. 2017;75(12):2599-2605.
[20] ALLEGRA A, OTERI G, ALONCI A, et al. Association of osteonecrosis of the jaws and POEMS syndrome in a patient assuming rituximab. J Craniomaxillofac Surg. 2014;42(4):279-282.
[21] GONZÁLEZ-OSUNA L, SIERRA-CRISTANCHO A, ROJAS C, et al. Premature Senescence of T-cells Favors Bone Loss During Osteolytic Diseases. A New Concern in the Osteoimmunology Arena. Aging Dis. 2021;12(5):1150-1161.
[22] LIU CG, LI DY, GAO X, et al. Examining the causal relationship between circulating immune cells and the susceptibility to osteomyelitis: A Mendelian randomization study. Int Immunopharmacol. 2024;131:111815.
[23] WANG C, ZHU Y, PAN D. Identifying the causal relationship between immune factors and osteonecrosis: a two-sample Mendelian randomization study. Sci Rep. 2024;14(1):9371.
[24] KUWAHARA N, KODAKA T, ZUSHI Y, et al. T-cell large granular lymphocytic (LGL) leukemia consists of CD4+/CD8dim and CD4-/CD8+ LGL populations in association with immune thrombocytopenia, autoimmune neutropenia, and monoclonal B-cell lymphocytosis. J Clin Exp Hematop. 2019;59(4):202-206.
[25] TAN Y, QIU Z, ZENG H, et al. Microcystin-leucine-arginine impairs bone microstructure and biomechanics by activating osteoimmune response and inhibiting osteoblasts maturation in developing rats. Toxicology. 2023;494:153595.
[26] EROGLU S, KARATAS G. Platelet/lymphocyte ratio is an independent predictor for osteoporosis. Saudi Med J. 2019;40(4):360-366.
[27] AKBAS EM, GUNGOR A, OZCICEK A, et al. Vitamin D and inflammation: evaluation with neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio. Arch Med Sci. 2016;12(4):721-727.
[28] MORRIS HA, TURNER AG, ANDERSON PPH. Vitamin-D regulation of bone mineralization and remodelling during growth. Front Biosci (Elite Ed). 2012;4(2): 677-689.
[29] RAMPOLDI F, DONATO E, ULLRICH L, et al. γδ T cells license immature B cells to produce a broad range of polyreactive antibodies. Cell Rep. 2022;39(8):110854.
[30] FRASE D, LEE C, NACHIAPPAN C, et al. The Inflammatory Contribution of B-Lymphocytes and Neutrophils in Progression to Osteoporosis. Cells. 2023; 12(13):1-15.
[31] LAGERQUIST MK, GUPTA P, SEHIC E, et al. Reduction of Mature B Cells and Immunoglobulins Results in Increased Trabecular Bone. JBMR Plus. 2022;6(9): e10670.
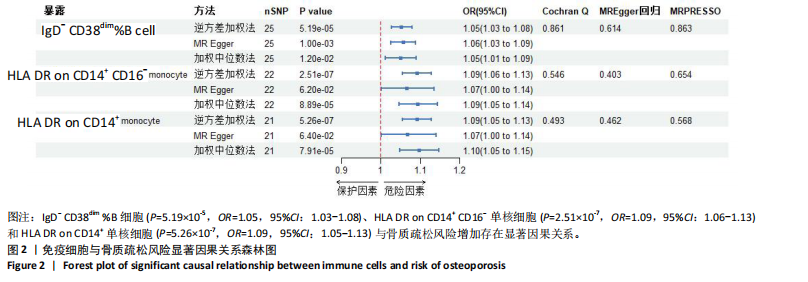
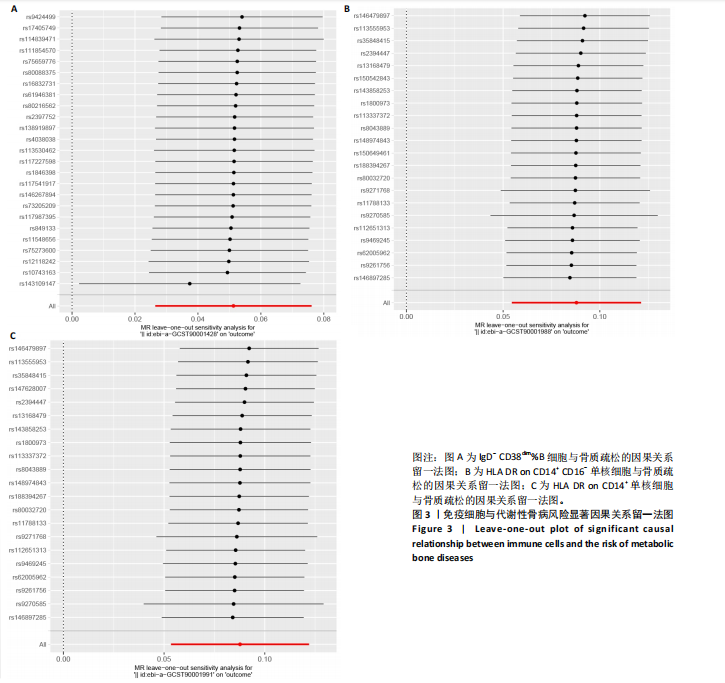
[32] DRUMMOND FJ, MACKRILL JJ, O’SULLIVAN K, et al. CD38 is associated with premenopausal and postmenopausal bone mineral density and postmenopausal bone loss. J Bone Miner Metab. 2006;24(1):28-35.
[33] BOLZONI M, TOSCANI D, COSTA F, et al. The link between bone microenvironment and immune cells in multiple myeloma: Emerging role of CD38. Immunol Lett. 2019;205:65-70.
[34] MAGGI J, CARRASCAL M, SOTO L, et al. Isolation of HLA-DR-naturally presented peptides identifies T-cell epitopes for rheumatoid arthritis. Ann Rheum Dis. 2022; 81(8):1096-1105.
[35] DOUROUDIS K, TARASSI K, ATHANASSIADES T, et al. HLA alleles as predisposal factors for postmenopausal osteoporosis in a Greek population. Tissue Antigens. 2007;69(6):592-596.
[36] TSUJI S, MUNKHBAT B, HAGIHARA M, et al. HLA-A*24-B*07-DRB1*01 haplotype implicated with genetic disposition of peak bone mass in healthy young Japanese women. Hum Immunol. 1998;59(4):243-249.
[37] LIN YC, ZHENG G, LIU HT, et al. USP7 promotes the osteoclast differentiation of CD14+ human peripheral blood monocytes in osteoporosis via HMGB1 deubiquitination. J Orthop Translat. 2023;40: 80-91.
[38] AMANO S, KAWAKAMI K, IWAHASHI H, et al. Functional role of endogenous CD14 in lipopolysaccharide-stimulated bone resorption. J Cell Physiol. 1997;173(3):301-309.
[39] COLLINS FL, STONE MD, TURTON J, et al. Oestrogen-deficiency induces bone loss by modulating CD14+ monocyte and CD4+ T cell DR3 expression and serum TL1A levels. BMC Musculoskelet Disord. 2019;20(1):326.
[40] KYRGIDIS A, YAVROPOULOU MP, ZIKOS P, et al Changes in peripheral monocyte populations 48-72 hours after subcutaneous denosumab administration in women with osteoporosis. J Musculoskelet Neuronal Interact. 2020;20(3):339-346.
[41] CAFIERO C, GIGANTE M, BRUNETTI G, et al. Inflammation induces osteoclast differentiation from peripheral mononuclear cells in chronic kidney disease patients: crosstalk between the immune and bone systems. Nephrol Dial Transplant. 2018;33(1):65-75.
[42] REINKE S, GEISSLER S, TAYLOR WR, et al. Terminally differentiated CD8⁺ T cells negatively affect bone regeneration in humans. Sci Transl Med. 2013;5(177): 177ra36.
[43] PIETSCHMANN P, GRISAR J, THIEN R, et al. Immune phenotype and intracellular cytokine production of peripheral blood mononuclear cells from postmenopausal patients with osteoporotic fractures. Exp Gerontol. 2001;36(10):1749-1759.
[44] SCHLUNDT C, REINKE S, GEISSLER S, et al. Individual Effector/Regulator T Cell Ratios Impact Bone Regeneration. Front Immunol. 2019;10:1954.
[45] OPELZ G, DÖHLER B. Association of mismatches for HLA-DR with incidence of posttransplant hip fracture in kidney transplant recipients. Transplantation. 2011;91(1):65-69.
[46] BAËHL S, GARNEAU H, LORRAIN D, et al. Alterations in Monocyte Phenotypes and Functions after a Hip Fracture in Elderly Individuals: A 6-Month Longitudinal Study. Gerontology. 2016;62(5):477-490.
[47] VIVEIROS MMH, VIVEIROS MEM, SILVA MG, et al. Expression of inflammatory cytokines in mesenchymal stem cells derived from proximal humerus fractures. Stem Cell Investig. 2022;9:3. |