[1] 陈生弟.中国帕金森病治疗指南(第三版)[J].中华神经科杂志,2014, 47(6):428-433.
[2] 张森,赵晓悦,梁宇,等.帕金森病致病因素及发病机制研究进展[J].药学学报,2020,55(10):2264-2272.
[3] NOH H, KWON S, CHO S, et al. Effectiveness and safety of acupuncture in the treatment of Parkinson’s disease: A systematic review and meta-analysis of randomized controlled trials. Complement Ther Med. 2017;34:86-103.
[4] 朱文昕,奚桂芳,睢久红.针药治疗对帕金森病小鼠脑内多巴胺影响[J].针刺研究,1996(4):46-49.
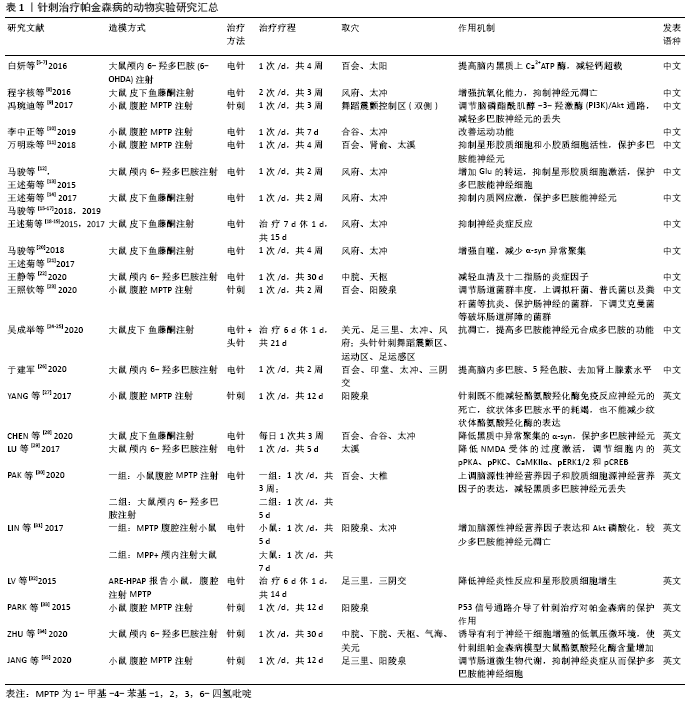
[5] 白妍,何便鸿,王东升,等.不同电针头穴透刺对PD大鼠不同时间点脑内黑质Ca~(2+)浓度的影响[J].中国中医药科技, 2016,23(2):180-181+236.
[6] 白妍,胡丙成,阿木拉,等.不同电针头穴透刺对PD大鼠脑内黑质Calbindin-D28k蛋白表达的影响[J].中国中医药科技, 2016,23(2):178-180.
[7] 白妍,卢金荣,胡丙成,等.不同电针头穴透刺对帕金森病大鼠脑内黑质钙稳态相关3种ATP酶活性的影响[J].中国中医药科技, 2016,23(1):4-5.
[8] 程宇核,张少武,朱小虎,等.电针对帕金森病模型大鼠黑质超氧阴离子、超氧化物岐化酶的影响[J].临床和实验医学杂志,2016,15(21): 2073-2076.
[9] 冯琬迪,王媛媛,盖聪,等.针刺联合美多芭对帕金森病小鼠脑多巴胺神经元及蛋白激酶B表达的影响[J].北京中医药大学学报,2017,40(3): 241-246.
[10] 李中正,盛益华,李思迪,等.电针对MPTP亚急性帕金森病模型小鼠步态运动行为的影响[J].湖南中医药大学学报,2019,39(7):874-878.
[11] 万明珠,任路,于嵩,等.“肾脑相济”电针疗法对帕金森病模型小鼠中脑黑质胶质细胞的影响[J].中医杂志,2018,59(18):1597-1601.
[12] 马骏,刘芳,王述菊,等.电针对帕金森病模型大鼠纹状体Glu浓度、GLT-1mRNA和GSmRNA表达的影响[J]. 时珍国医国药,2015,26(12): 3050-3053.
[13] 王述菊,马骏,刘芳,等.电针对帕金森病模型大鼠纹状体Glu浓度、GS和PAG表达的影响[J].世界科学技术-中医药现代化,2015,17(10): 2079-2082.
[14] 王述菊,王中明,马骏,等.电针对帕金森病模型大鼠黑质内质网应激相关基因表达的影响[J].时珍国医国药,2017,28(6):1497-1500.
[15] 马骏,王彬,王述菊,等.电针“风府、太冲”穴对帕金森病模型大鼠内质网应激相关蛋白表达的影响[J].中国康复医学杂志,2019,34(7): 772-777.
[16] 马骏,王中明,王述菊,等.电针对帕金森病模型大鼠黑质内Bip、CHOP蛋白表达的影响[J].上海针灸杂志,2018,37(1):86-91.
[17] 马骏,袁利,王述菊,等.电针对帕金森病大鼠中脑黑质转录活化因子6和转录因子X盒结合蛋白1 mRNA表达的影响[J].针刺研究,2019, 44(11):805-809.
[18] 王述菊,马骏,王彦春,等.电针对鱼藤酮诱导的帕金森病模型大鼠黑质内ERK1/2及TNF-α的影响[J].中国老年学杂志,2015,35(20):5694-5697.
[19] 王述菊,马骏,王彦春,等.电针对帕金森病模型大鼠黑质区c-Jun氨基末端激酶和TNF-α、IFN-γ、IL-1β蛋白表达的影响[J].中华中医药学刊, 2017,35(1):43-46.
[20] 马骏,余沛豪,王述菊,等.电针对帕金森病模型大鼠脑黑质内Lamp2a、 Hsc70、α-syn表达的影响[J].中华中医药学刊,2018,36(4):859-862.
[21] 王述菊,余沛豪,马骏,等.电针对鱼藤酮诱导的帕金森病模型大鼠黑质内自噬相关蛋白表达的影响[J].辽宁中医杂志,2017,44(9):1812-1815.
[22] 王静,王安龙,范小明,等.经颅超声对电针治疗帕金森病模型大鼠的效果评价[J].中华医学超声杂志(电子版),2020,17(1):70-75.
[23] 王照钦,钟蕊,高崚,等.针刺对帕金森病模型小鼠肠道菌群多样性的调节作用[J].中华中医药杂志,2020,35(5):2265-2270.
[24] 吴成举,英锡相,陈靖,等.针刺疗法对帕金森病大鼠黑质神经元凋亡蛋白bcl-2、bax的影响[J].陕西中医,2020,41(1):8-11+133.
[25] 吴成举,英锡相,马贤德,等.不同方法针灸对帕金森模型大鼠脑细胞神经元代谢影响[J].辽宁中医药大学学报,2020,22(6):12-15.
[26] 于建军.电针对帕金森抑郁模型大鼠脑内单胺类神经递质含量影响研究[J].针灸临床杂志,2020,36(2):70-73.
[27] YANG HJ, GAO Y, YUN JY, et al. Acupuncture does not protect against 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced damage of dopaminergic neurons in a preclinical mouse model of Parkinson’s disease. Neuroreport. 2017;28(1):50-55.
[28] CHEN LD, CHEN K, AI L,et al. Effect of electroacupuncture on dopaminergic neurons in a rat model of Parkinson’s disease based on the alpha-synuclein pathway. Mater Express. 2020;10(1):62-69.
[29] LU KW, YANG J, HSIEH CL, et al. Electroacupuncture restores spatial learning and downregulates phosphorylated N-methyl-D-aspartate receptors in a mouse model of Parkinson’s disease. Acupunct Med. 2017;35(2):133-141.
[30] PAK ME, AHN SM, JUNG DH, et al. Electroacupuncture Therapy Ameliorates Motor Dysfunction via Brain-Derived Neurotrophic Factor and Glial Cell Line-Derived Neurotrophic Factor in a Mouse Model of Parkinson’s Disease. J Gerontol A Biol Sci Med Sci. 2020;75(4):712-721.
[31] LIN JG, CHEN CJ, YANG HB, et al. Electroacupuncture Promotes Recovery of Motor Function and Reduces Dopaminergic Neuron Degeneration in Rodent Models of Parkinson’s Disease. Int J Mol Sci. 2017;18(9):1846.
[32] LV E, DENG J, YU Y, et al. Nrf2-ARE signals mediated the anti-oxidative action of electroacupuncture in an MPTP mouse model of Parkinson’s disease.Free Radic Res. 2015;49(11):1296-307.
[33] PARK JY, CHOI H, BAEK S, et al. p53 signalling mediates acupuncture-induced neuroprotection in Parkinson’s disease.Biochem Biophys Res Commun. 2015;460(3):772-779.
[34] ZHU LS, WANG J, LU J, et al. Effect of hemodynamic characteristic changes of the carotid artery on 6-OHDA-induced Parkinson’s disease model rats treated by Gut-acupuncture.Journal of King Saud University - Science. 2020; 32(6):2675-2681.
[35] JANG JH, YEOM MJ, AHN S, et al. Acupuncture inhibits neuroinflammation and gut microbial dysbiosis in a mouse model of Parkinson’s disease. Brain Behav Immun. 2020;89:641-655.
[36] Aron L,Klein R.Repairing the parkinsonian brain with neurotrophic factors.Trends Neurosci. 2011;34(2):88-100.
[37] NASROLAHI A, MAHMOUDI J, AKBARZADEH A, et al. Neurotrophic factors hold promise for the future of Parkinson’s disease treatment: is there a light at the end of the tunnel? Rev Neurosci. 2018;29(5):475-489.
[38] GILL SS, PATEL NK, HOTTON GR, et al.Direct brain infusion of glial cell line-derived neurotrophic factor in Parkinson disease. Nat Med. 2003;9(5):589-595.
[39] PENG C, ARON L, KLEIN R, et al. Pitx3 is a critical mediator of GDNF-induced BDNF expression in nigrostriatal dopaminergic neurons.J Neurosci. 2011;31(36):12802-12815.
[40] SALVATORE MF, DAVIS RW, ARNOLD JC, et al.Transient striatal GLT-1 blockade increases EAAC1 expression, glutamate reuptake, and decreases tyrosine hydroxylase phosphorylation at ser(19). Exp Neurol. 2012;234(2):428-436.
[41] 李敬军,马羽,胡文瀚,等.丘脑底核高频电刺激对偏侧帕金森猴苍白球内侧部中氨基酸神经递质含量的影响[J].立体定向和功能性神经外科杂志,2012,25(2):68-71.
[42] 邓娟,白洁.TRPC1和Ca~(2+)在帕金森病内质网应激中的作用[J].生命科学,2012,24(10):1169-1173.
[43] MOCHIZUKI H, GOTO K, MORI H, et al. Histochemical detection of apoptosis in Parkinson’s disease. J Neurol Sci. 1996;137(2):120-123.
[44] 钟河江,杨天德.内质网应激与免疫炎症反应的研究进展[J].重庆医学, 2012,41(2):201-203+206.
[45] TAKAYANAGI S, FUKUDA R, TAKEUCHI Y,et al.Gene regulatory network of unfolded protein response genes in endoplasmic reticulum stress.Cell Stress Chaperones. 2013;18(1):11-23.
[46] 陈欢.氯胺酮诱导PC12细胞凋亡的内质网应激机制研究[D].石家庄:河北医科大学,2014.
[47] MCCULLOUGH K, MARTINDALE J, KLOTZ L,et al. Gadd153 sensitizes cells to endoplasmic reticulum stress by down-regulating Bcl2 and perturbing the cellular redox state.Mol Cell Biol. 2001;21(4):1249-1259.
[48] 马骏,王中明,王述菊,等.电针对帕金森病模型大鼠内质网应激IRE1α-ASK1-JNK通路的影响[J].中国康复医学杂志,2018,33(6):658-662+680.
[49] CRUZ J, TSAI L. Cdk5 deregulation in the pathogenesis of Alzheimer’s disease. Trends Mol Med. 2004;10(9):452-458.
[50] MORSELLI E, MARIÑO G, BENNETZEN M, et al.Spermidine and resveratrol induce autophagy by distinct pathways converging on the acetylproteome. J Cell Biol. 2011;192(4):615-629.
[51] 刘康永,石际俊,倪夏珺,等.α-核突触蛋白和自噬在帕金森病中的作用[J].中国临床神经科学,2010,18(1):103-107.
[52] MASSEY AC, KAUSHIK S, SOVAK G,et al.Consequences of the selective blockage of chaperone-mediated autophagy. Proc Natl Acad Sci U S A. 2006;103(15):5805-5810.
[53] LI D, SHI JJ, MAO CJ, et al.Alteration of dynein function affects α-synuclein degradation via the autophagosome-lysosome pathway. Int J Mol Sci. 2013; 14(12):24242-24254.
[54] SHEN YF, TANG Y, ZHANG XJ,et al.Adaptive changes in autophagy after UPS impairment in Parkinson’s disease. Acta Pharmacol Sin. 2013;34(5):667-673.
[55] Whitton P. Inflammation as a causative factor in the aetiology of Parkinson’s disease. Br J Pharmacol. 2007;150(8):963-976.
[56] MORGANTI-KOSSMANN M, SATGUNASEELAN L, BYE N, et al: Modulation of immune response by head injury. Injury. 2007;38(12):1392-1400.
[57] 吕风月,赵咏梅.星形胶质细胞在帕金森病发病机制中的作用[J].基础医学与临床,2008,28(5):516-518.
[58] 庄文欣,付文玉,吕娥,等.帕金森病大鼠黑质小胶质细胞及星形胶质细胞的变化[J].解剖学报,2010,41(3):344-348.
[59] 马骏,马彪,王述菊,等.电针对帕金森病大鼠纹状体缝隙连接蛋白43的表达及谷氨酸含量的影响[J].针刺研究,2015,40(5):364-367+372.
[60] Visanji NP, Brooks PL, Hazrati LN,et al.The prion hypothesis in Parkinson’s disease: Braak to the future. Acta Neuropathol Commun. 2013;1:2.
[61] Sampson TR, Debelius JW, Thron T,et al.Gut Microbiota Regulate Motor Deficits and Neuroinflammation in a Model of Parkinson’s Disease.Cell. 2016;167(6):1469-1480.e12.
[62] Kim S, Kwon SH, Kam TI, et al.Transneuronal Propagation of Pathologic α-Synuclein from the Gut to the Brain Models Parkinson’s Disease. Neuron. 2019;103(4):627-641.e7.
[63] 杨东明,杨利峰,赵德明,等.帕金森病动物模型的研究进展[J].中国实验动物学报,2020,28(3):397-404.
[64] 陈蕾蕾,宋宁,谢俊霞.黑质铁沉积致帕金森病的机制研究进展[J].青岛大学学报(医学版),2020, 56(2):127-132.
[65] 赵喆,鲍秀琦,张丹.铁死亡调控机制及其在帕金森病中的研究进展[J].药学学报,2019,54(3):399-406. |