中国组织工程研究 ›› 2016, Vol. 20 ›› Issue (21): 3117-3123.doi: 10.3969/j.issn.2095-4344.2016.21.011
• 细胞外基质材料 extracellular matrix materials • 上一篇 下一篇
脱细胞羊膜与医用膜修复腱鞘缺损防治肌腱粘连的比较
刘国立,于昆仑,白江博,马 韬,杨彦涛,田德虎
- 河北医科大学第三医院,河北省石家庄市 050000
Acellular amniotic membrane versus medical membrane to prevent tendon adhesion in tendon sheath repair
Liu Guo-li, Yu Kun-lun, Bai Jiang-bo, Ma Tao, Yang Yan-tao, Tian De-hu
- (the Third Hospital of Hebei Medical University, Shijiazhuang 050000, Hebei Province, China
摘要:
文章快速阅读:
.jpg)
文题释义: 脱细胞羊膜:是经处理后的羊膜,去除上皮细胞层,仅有基底膜,因其组织相容性好,抗原性低,无毒副作用,在体内可被降解,在烧伤、眼科、妇产等领域等到了广泛应用。如 Gris等报道了冻干羊膜在眼科疾病治疗方面的作用,患者在随访中无不良反应;董丽霞等成功完成羊膜移植阴道成形37例,术后35例获随访,效果均满意。 理想的腱鞘修补材料:①可被吸收,在体内不残留任何异物。②获取容易,组织相容性好,无局部及全身无不良反应。③具有良好的通透性,在阻断肌腱外源性愈合的同时不影响肌腱愈合质量。④最好含有促进细胞黏附、生长、增殖和分化的因子。
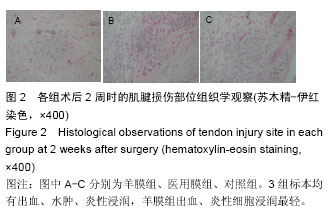
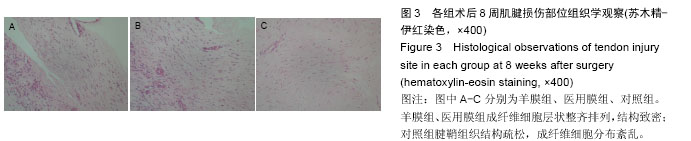
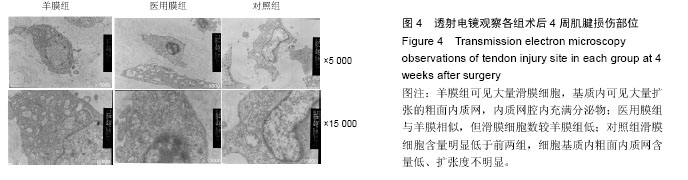
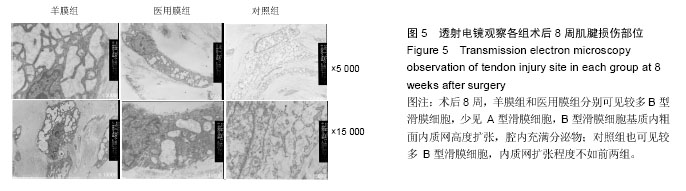
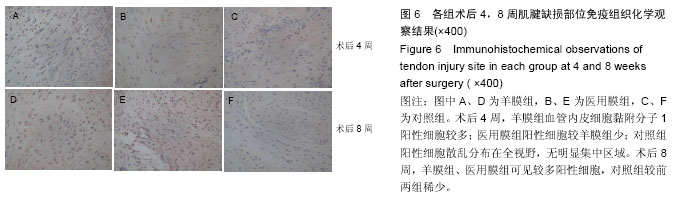
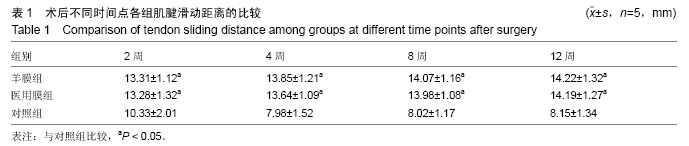
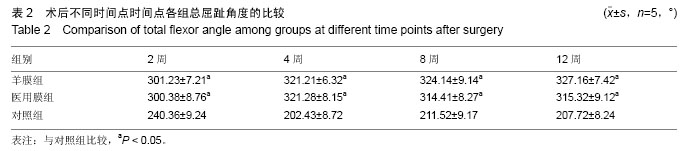
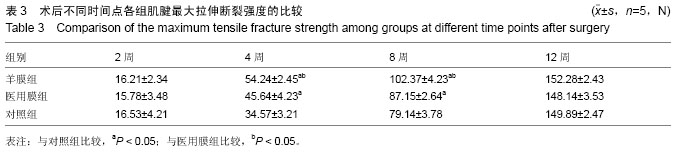
背景:实验证实生物膜可用于腱鞘缺损的重建,抑制肌腱外源性愈合,为肌腱滑动提供良好的基床,减轻肌腱粘连。 目的:比较脱细胞羊膜与医用膜修复腱鞘缺损中防治肌腱粘连的作用。 方法:于66只来亨鸡双足第Ⅲ趾制备肌腱损伤、腱鞘缺损模型,随机分为3 组,每组22只,羊膜组采用脱细胞羊膜修复腱鞘缺损,医用膜组采用可吸收医用膜修复腱鞘缺损,对照组不修复腱鞘。术后2,4,8,12周取各组标本,进行大体、组织学及生物力学检测。 结果与结论:①大体观察:术后12周,羊膜组、医用膜组腱鞘完整,肌腱愈合良好,无粘连;对照组肌腱粘连严重。②组织学:术后8周,羊膜组假鞘中滑膜细胞数最多,基质内粗面内质网高度扩张,分泌旺盛,医用膜组次之,对照组滑膜细胞数最少,分布杂乱,基质内扩张空泡较前两组弱。术后12 周羊膜组、医用膜组成纤维细胞层状整齐排列,结构致密;对照组腱鞘组织结构疏松,成纤维细胞分布絮乱。③生物力学:羊膜组、医用膜组肌腱滑动距离、总屈趾角度均大于对照组(P < 0.05),前两组间比较差异无显著性意义。术后12周,3组间最大拉伸断裂强度比较差异无显著性意义。④结果表明,脱细胞羊膜与医用膜重建腱鞘缺损均能明显屏障肌腱外源性愈合,防治肌腱粘连。
ORCID: 0000-0002-9024-1654(田德虎)
中图分类号:

.jpg)