[1] METZ R, KERKHOFFS GM, VERLEISDONK EJ, et al. Acute Achilles tendon rupture: minimally invasive surgery versus non operative treatment, with immediate full weight bearing. Design of a randomized controlled trial. BMC Musculoskelet Disord. 2007;8:108.
[2] DE JONG JP, NGUYEN JT, SONNEMA AJ, et al. The incidence of acute traumatic tendon injuries in the hand and wrist: a 10-year population-based study. Clin Orthop Surg. 2014;6(2):196-202.
[3] DY CJ, HERNANDEZ-SORIA A, MA Y, et al. Complications after flexor tendon repair: a systematic review and meta-analysis. J Hand Surg Am. 2012;37(3):543-551
[4] 赵颂,童致虹,梁海东,等.防治肌腱粘连的研究进展[J].实用手外科杂志,2013,27(1):60-63,67.
[5] TAN V, NOURBAKHSH A, CAPO J, et al. Effects of nonsteroidal anti-inflammatory drugs on flexor tendon adhesion. J Hand Surg Am. 2010;35(6):941-947.
[6] KHANNA A, FRIEL M, GOUGOULIAS N, et al. Prevention of adhesions in surgery of the flexor tendons of the hand: what is the evidence. Br Med Bull. 2009;90:85-109.
[7] OZBÖLÜK S, OZKAN Y, OZTÜRK A, et al. The effects of human amniotic membrane and periosteal autograft on tendon healing: experimental study in rabbits. J Hand Surg Eur Vol. 2010;35(4):262-268.
[8] KING AE, PALTOO A, KELLY RW, et al. Expression of natural antimicrobials by human placenta and fetal membranes. Placenta. 2007;28(2-3):161-169.
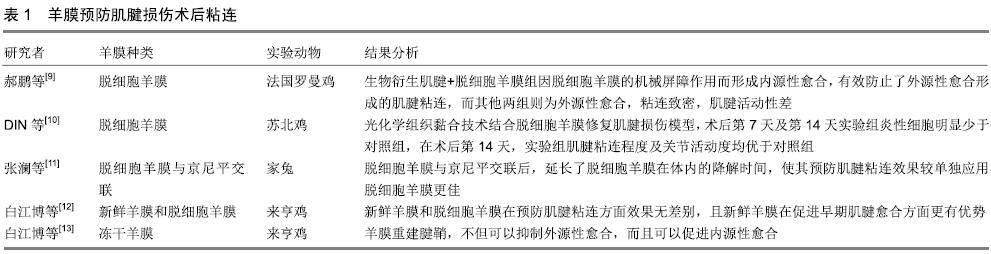
[9] 郝鹏,项舟,罗静聪,等.脱细胞羊膜预防生物衍生肌腱修复鸡屈趾肌腱Ⅱ区缺损修复后的粘连[J].中国组织工程研究与临床康复, 2011,15(34):6355-6359.
[10] DING B, WANG X, YAO M. Photochemical Tissue Bonding Technique for Improving Healing of Hand Tendon Injury. Surg Innov. 2019;26(2):153-161.
[11] 张澜.京尼平交联脱细胞羊膜预防兔跟腱粘连[J].世界最新医学信息文摘(连续型电子期刊),2015(64):105-108.
[12] 白江博,赵红芳,高瑞姣,等.新鲜羊膜与脱细胞羊膜修复腱鞘缺损预防肌腱粘连[J].中国组织工程研究,2017,21(30): 4842-4846.
[13] 白江博,赵红芳,张冰,等.冻干羊膜重建腱鞘缺损对肌腱愈合的早期生物力学影响[J].河北医科大学学报,2018,39(1):34-38.
[14] 张乐,崔树森,杨光,等.纳米化姜黄素抑制大鼠跟腱粘连的实验研究[J].中华手外科杂志,2016,32(2):141-144.
[15] 李鹏昊,刘舒云,郭全义.肌腱断裂修补术后药物预防腱周粘连的研究进展[J].中国医药生物技术,2017,12(2):162-165.
[16] 张鹏.肌腱损伤局部置入链霉素复合缓释降解膜的实验研究[D].长春:吉林大学,2008.
[17] HUNG LK, FU SC, LEE YW, et al. Local vitamin-C injection reduced tendon adhesion in a chicken model of flexor digitorum profundus tendon injury. J Bone Joint Surg Am. 2013;95(7):e41.
[18] 周智,左文山,谢跃,等.5-氟尿嘧啶联合大清止血膜预防肌腱粘连的临床研究[J].疑难病杂志,2014,13(3):291-293.
[19] LOISELLE AE, FRISCH BJ, WOLENSKI M, et al. Bone marrow-derived matrix metalloproteinase-9 is associated with fibrous adhesion formation after murine flexor tendon injury. PLoS One. 2012;7(7):e40602.
[20] XIA C, ZUO J, WANG C, et al. Tendon healing in vivo: effect of mannose-6-phosphate on flexor tendon adhesion formation. Orthopedics. 2012;35(7):e1056-1060.
[21] CHEN Q, LU H, YANG H. Chitosan inhibits fibroblasts growth in Achilles tendon via TGF-β1/Smad3 pathway by miR-29b. Int J Clin Exp Pathol. 2014;7(12):8462-8470.
[22] CHEN Q, LU H, YANG H. Chitosan prevents adhesion during rabbit flexor tendon repair via the sirtuin 1 signaling pathway. Mol Med Rep. 2015;12(3):4598-4603.
[23] JIANG K, CHUN G, WANG Z, et al. Effect of transforming growth factor-β3 on the expression of Smad3 and Smad7 in tenocytes. Mol Med Rep. 2016;13(4):3567-3573.
[24] YURDAKUL SIKAR E, SIKAR HE, TOP H, et al. Effects of Hyalobarrier gel and Seprafilm in preventing peritendinous adhesions following crush-type injury in a rat model. Ulus Travma Acil Cerrahi Derg. 2019;25(2):93-98.
[25] 王晓龙.几丁糖(壳聚糖)对兔肩袖损伤术后粘连的预防及组织学研究[D].青岛:青岛大学,2018.
[26] 李鹏昊,刘舒云,王亚洁,等.电纺聚乳酸-羟基乙酸共聚物/Ⅰ型胶原-聚己内酯双层膜预防腱周粘连的相关研究[J].中国医药生物技术,2017,12(4):289-296.
[27] YOSHIKAWA Y, ABRAHAMSSON SO. Dose-related cellular effects of platelet-derived growth factor-BB differ in various types of rabbit tendons in vitro. Acta Orthop Scand. 2001; 72(3):287-292.
[28] 林樾.血小板源性生长因子BB促进大鼠肌腱愈合和防止肌腱粘连的作用和机制[D]. 南京:南京大学,2010.
[29] 何爱咏,莫挺挺.血管内皮生长因子对免跟腱内源性愈合作用的量效关系[J].中国组织工程研究与临床康复, 2009,13(37): 7335-7340.
[30] 徐红立,王士娥,王子明,等.血管内皮生长因子中和抗体对屈肌腱粘连的影响[J].中华手外科杂志,2007,23(4):237-240.
[31] 柯尊山,汤锦波.损伤后肌腱及粘连组织中五种生长因子基因的表达及意义[J].中华创伤骨科杂志,2007,9(4):345-348.
[32] RAGHAVAN SS, WOON CY, KRAUS A, et al. Optimization of human tendon tissue engineering: synergistic effects of growth factors for use in tendon scaffold repopulation. Plast Reconstr Surg. 2012;129(2):479-489.
[33] CHEN CH, CAO Y, WU YF, et al. Tendon healing in vivo: gene expression and production of multiple growth factors in early tendon healing period. J Hand Surg Am. 2008;33(10): 1834-1842.
[34] THOMOPOULOS S, DAS R, SAKIYAMA-ELBERT S, et al. bFGF and PDGF-BB for tendon repair: controlled release and biologic activity by tendon fibroblasts in vitro. Ann Biomed Eng. 2010;38(2):225-234.
[35] 沙德峰,辛畅泰,杨晓霞,等.肌腱损伤缝接处置入碱性成纤维细胞生长因子复合缓释降解膜的研究[J].中国修复重建外科杂志, 2004,18(2):148-151.
[36] TANG JB, CAO Y, ZHU B, et al. Adeno-associated virus-2-mediated bFGF gene transfer to digital flexor tendons significantly increases healing strength. an in vivo study. J Bone Joint Surg Am. 2008;90(5):1078-1089.
[37] TSUZAKI M, BRIGMAN BE, YAMAMOTO J, et al. Insulin-like growth factor-I is expressed by avian flexor tendon cells. J Orthop Res. 2000;18(4):546-556.
[38] 任强,黄昌林,郭振海.兔跟腱修复过程中胰岛素样生长因子-Ⅰ的表达[J].郑州大学学报(医学版),2005,40(6):1067-1069.
[39] XIA CS, ZUO AJ, WANG CY, et al. Isolation of rabbit bone marrow mesenchymal stem cells using density gradient centrifugation and adherence screening methods. Minerva Med. 2013;104(5):519-525.
[40] 夏长所,洪光祥,张才龙,等.肌腱愈合过程中转化生长因子β1基因表达的变化[J].中国修复重建外科杂志,2007,21(9):975-978.
[41] 张志敏,刘建,吴尧平,等. TGFβ1抗体复合生物蛋白胶预防术后肌腱粘连[J].第四军医大学学报,2008,29(1):70-73.
[42] WU YF, MAO WF, ZHOU YL, et al. Adeno-associated virus-2-mediated TGF-β1 microRNA transfection inhibits adhesion formation after digital flexor tendon injury. Gene Ther. 2016;23(2):167-175.
[43] FUJIHARA Y, OTA H, WATANABE K. Utility of early active motion for flexor tendon repair with concomitant injuries: A multivariate analysis. Injury. 2018;49(12):2248-2251.
[44] WALLACE SJ, MIOTON LM, HAVEY RM, et al. Biomechanical Properties of a Novel Mesh Suture in a Cadaveric Flexor Tendon Repair Model. J Hand Surg Am. 2019;44(3):208-215.
[45] MENG J, YU P, TONG J, et al. Hydrogen treatment reduces tendon adhesion and inflammatory response. J Cell Biochem. 2018 Oct 26. doi: 10.1002/jcb.27441. [Epub ahead of print]
[46] LIPAR M, ZDILAR B, KRESZINGER M, et al. Extracellular matrix supports healing of transected rabbit Achilles tendon. Heliyon. 2018;4(9):e00781.
[47] PAOLIN A, TROJAN D, LEONARDI A, et al. Cytokine expression and ultrastructural alterations in fresh-frozen, freeze-dried and γ-irradiated human amniotic membranes. Cell Tissue Bank. 2016;17(3):399-406.
[48] MOHAN R, BAJAJ A, GUNDAPPA M. Human Amnion Membrane: Potential Applications in Oral and Periodontal Field. J Int Soc Prev Community Dent. 2017;7(1):15-21.
[49] FAVARON PO, CARVALHO RC, BORGHESI J, et al. The Amniotic Membrane: Development and Potential Applications-A Review. Reprod Domest Anim. 2015;50(6):881-892.
[50] PETERSEN W, PUFE T, KURZ B, et al. Angiogenesis in fetal tendon development: spatial and temporal expression of the angiogenic peptide vascular endothelial cell growth factor. Anat Embryol (Berl). 2002;205(4):263-270.
|